I was reviewing a report recently that included the results for walking oximetry. These showed that the individual has a resting SaO2 of 97% and desaturated significantly to 86% after walking a couple hundred yards. This was curious since a DLCO had also been performed and the results for that test were 94% of predicted. It’s unusual for somebody with a normal DLCO to have that low of an SaO2 but I have seen it before in individuals who were unable to ventilate adequately because of a paralyzed diaphragm. I’ve also seen it happen sometimes when somebody has a peripheral vascular disease like Reynaud’s that produces a poor quality oximeter signal. Buried in the technician’s notes however, was an additional piece of information that called into question both the resting and the exercise SaO2 readings. Specifically, the notes mentioned that an ABG had been performed and that the subject’s COHb was 9%.
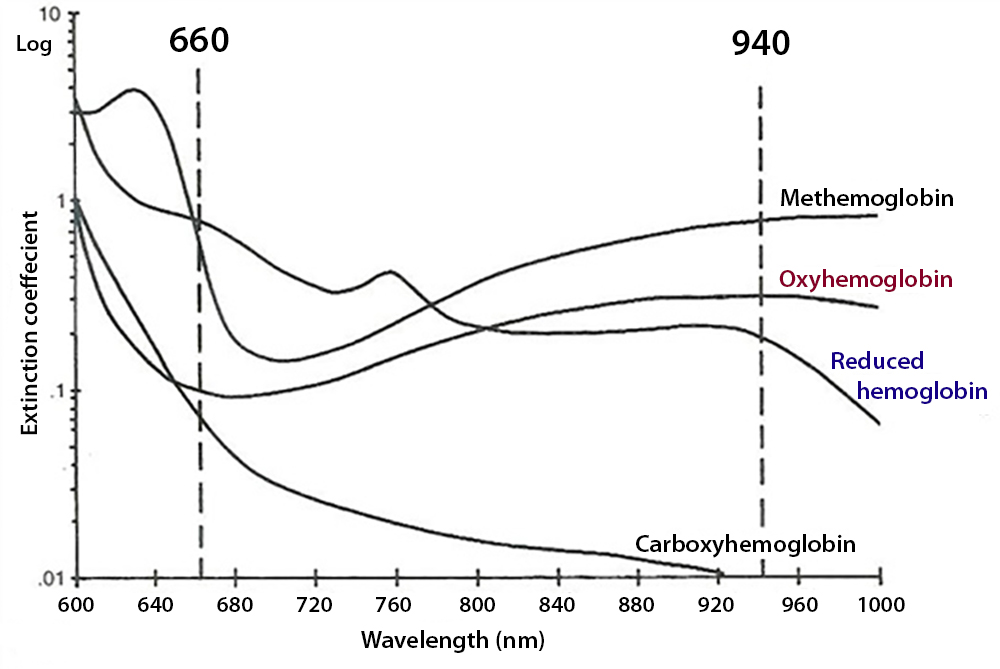
Oxygen saturation is measured spectrophotometrically. The different forms of hemoglobin, i.e. oxyhemoglobin (O2Hb), deoxyhemoglobin, methemoglobin (MetHb) and carboxyhemoglobin (COHb) absorb the frequencies of red and infrared light differently.
Although non-invasive oximetry was first developed during the 1930’s and 1940’s (in 1935 by K. Mathes in Germany and independently in 1942 by G. Milliken in the USA), current pulse oximeter technology dates from 1972 (by Takuo Aoyagi, researcher for Nihon Koden in Japan). The original pulse oximeters were large, bulky and generally stationary pieces of equipment. Oximeters underwent progressive miniaturization during the 1980’s and 1990’s and rapidly evolved into the handheld and fingertip units we see today and the only “stationary” oximeters that remain are those used in ICU-type monitoring systems.
Modern laboratory CO-oximeters measure the absorption of light in a blood sample at up to 128 wavelengths, spread across the entire hemoglobin absorption spectrum. Using mathematical analysis they can report total hemoglobin concentration and oxygen saturation in addition to fractional deoxyhemoglobin, COHb, and MetHb.
A pulse oximeter however, transmits only two wavelengths of light through tissue, typically 660 and 940 nm. Body tissue contains both arterial and venous blood and a pulse oximeter differentiates between these by using the cyclical rise and fall of overall light absorption that occurs because of the heart beat. The majority of light absorbed during pulse oximetry is due to skin, connective tissue, bone and venous blood and this does not change during the cardiac cycle. Arterioles however, contain more blood during systole than they do during diastole and by comparing the peak to the trough the light absorption by non-arterial sources becomes irrelevant.
Although the mathematics are more complex than this, it is primarily the ratio of light absorbed at 660 nm (red) to that at 940 nm that in turn is used to perform a look-up from a table of empirically derived values in order to calculate SaO2.
It has long been known that pulse oximeters are insensitive to carbon monoxide. The reason for this is that COHb and O2Hb have similar absorbances at 660 nm and this results in pulse oximeters measuring COHb and O2Hb similarly. Although the absorbances of COHb and O2Hb somewhat differ at 990 nm this does not become apparent until COHb is approximately 40% or greater. Up until the higher levels of COHb are reached the SaO2 reported by a pulse oximeter is usually equal to SaO2 + COHb.
A rule of thumb for oximeters (whether non-invasive or not) is that the number of forms of hemoglobin that can be measured is equal to the number of wavelengths that are measured. This means that oximeters that measure light at two wavelengths can only measure O2Hb and de-oxygenated Hb. Pulse oximeters that measured additional light wavelengths and considered capable of measuring COHb (as well as hemoglobin and methemoglobin) were first developed and manufactured around 2005. Unfortunately, as useful as a pulse CO-oximeter might be their accuracy and reliability remains questionable. Verification this type of pulse oximeter has shown equivocal results. For every research study that has shown good agreement with a laboratory-based CO-oximeter there is another that showed poor correlation instead. On a positive note however, one study showed that although there were significant differences in measured COHb between pulse oximetry and laboratory CO-oximetry, the initial finding of elevated COHb levels in the emergency room lead to significantly quicker treatment.
What the COHb of 9% told me was that the baseline SaO2 of 97% was inaccurate since the highest that the SaO2 could really have been was 91%. It’s also unclear how accurate the exercise SaO2 of 86% was. When I looked up this individual’s ABG results their resting SaO2 measured on a laboratory CO-oximeter was actually 81%, which means that all of the oximeter readings were incorrect.
Although the oximeter reading were incorrect, does that also mean that the significant desaturation during exercise actually occurred? There’s no way to be sure but given how a pulse oximeter works I’m going to say that it probably did.
Pulse oximetry has been called the “fifth vital sign” (although pain has been called that as well) and seems to be responsible for a significant decrease in clinical use of ABGs. As an example my lab (which sees outpatients almost exclusively) is currently performing about half the number of ABG’s per year that we did in the 1990’s and the total number of patients seen in my lab is about double from then. In one sense this a good thing, but a problem with it is that the other ABG values such as PaCO2, pH and COHb, which are often more clinically relevant to patients with COPD, aren’t being performed as often as they should be.
Oximetry is frequently used during CPETs, 6-minute walk studies and walking oximetry. A number of studies have shown that pulse oximetry during exercise both over- and underestimates oxygen saturation when compared to arterial samples measured on a CO-oximeter, but not predictably so. In addition, oximetry during field testing (6MWT, walking oximetry) is subject to motion artifact and operator errors.
A prime example of an operator error that we saw a couple of years ago was a young woman who had recently delivered a baby. Her obstetrician had made an “emergency” PFT appointment for her because despite having no symptoms she desaturated into the upper 70’s while doing a walking oximetry test in the physician’s office. At our lab she had normal PFTs and normal walking oximetry and while talking to her, I found that she had been carrying her baby while walking and that the oximeter probe had been placed on a finger of the hand she was using to carrying her baby.
Along the same lines, I’ve seen nursing assistants place the oximeter probe on a finger of the same arm they’re using to take blood pressures and then document the low SaO2 that occurred while the blood pressure cuff was pumped up (this happened to my wife during a routine clinic visit). I’d like to say that my lab’s technicians wouldn’t make a similar error but I’ve seen our staff place the oximeter probe on a finger of the hand that a mobility-impaired patient was using to hold their cane.
But more importantly I think that we seem to have forgotten about oximetry’s inherent limitations. Numerous studies have shown that pulse oximetry correlates well with SaO2 measured by CO-oximetry, but correlation doesn’t necessarily mean accuracy. The accuracy of pulse oximeters has been shown to vary somewhat by manufacturer and ranges from +/- 3% to +/- 5% (which is somewhat in contrast to general manufacturer claims of +/-2% accuracy). In addition, pulse oximetry accuracy is highest at SaO2s of between 82% to 94%, and much less so outside of that range. Interestingly, despite anecdotal evidence to the contrary, a couple of studies have shown that skin pigmentation and nail polish do not affect overall oximeter accuracy.
There are still a large number of smokers around, and pulmonary labs probably see a higher percentage of them than what’s in the general population. The average COHb levels of smokers is 3% to 5% but as a general rule COHb rises by approximately 5% for every pack of cigarettes smoked per day so higher levels are not only possible but in many cases highly probable. Elevated COHb levels are important for numerous clinical (and technical) reasons but in most cases we don’t know what an individual’s COHb level is because (at least for my lab) it requires an arterial puncture. Pulse oximetry has shown itself to be incredibly useful but in order to use it properly we have to remember its limitations.
References:
Adler JN, Hughes LA, Vivilecchia R, Camargo CA. Effect of skin pigmentation of pulse oximetry accuracy in the emergency department. Acad Emerg Med 1998; 5: 965-970.
Amalakanti S, Pentakota MR. Pulse oximetry overestimates oxygen saturation in COPD. Resp Care 2016; 61(4): 423-427.
Barker SJ, Shah NK. The effects of motion on the performance of pulse oximeters in volunteers. Anesthesiology 1997; 86(1): 101-108.
Barker SJ, Curry J, Redford D, Morgan S. Measurement of carboxyhemoglobin and methemoglobin by pulse oximetry. Anesthesiology 2006; 105: 892-897.
Bozeman WP, Myers RAM, Barish RA. Confirmation of the pulse oximetry gap in carbon monoxide poisoning. Ann Emerg Med 1997; 30(5): 608-611.
Chan ED, Chan MM, Chan MM. Pulse oximetry: Understanding its basic principals facilitates appreciation of its limitations. Resp Med 2013; 107: 789-799.
Chiappini F, Fuso L, Pistelli R. Accuracy of a pulse oximeter in the measurement of oxyhaemoglobin saturation. Eur Respir J 1998; 11: 716-719.
Coulange M, Barthelemy A, Hug F, Thierry AL, De Haro L. Reliability of new pulse CO-oximeter in victims of carbon monoxide poisoning. Undersea Hyperbaric Medicine 2008; 35(2): 107-111.
Diaz-Gonzalez CDLM, Hormiga MDLR, Lopez JMR, Rivero YD, Morales MSM. Concordance among measurements obtained by three pulse oximeters currently used by health professionals. J Clin Diag Res 2014; 8(8): MC09-MC12.
Hampson NH. Pulse oximetry in severe carbon monoxide poisoning. Chest 1998; 114: 1036-1041.
Hampson NH, Exker ED, Scott KL. Use of a noninvasive pulse Co-Oximeter to measure blood carboxyhemoglobin levels in bingo players. Resp Care 2006; 51(7): 758-760.
Hampson NH. Noninvasive pulse CO-oximetry expedites evaluation and management of patients with carbon monoxide poisoning. J Emerg Med 2012; 30: 2021-2024.
Hampson NH, Piantodosi CA, Thom SR, Weaver LK. Concise Clinical Review. Practice recommendations in the diagnosis, management and prevention of carbon monoxide poisoning. Amer J Respir Crit Care Med 2012; 186(11): 1095-1101.
Hannhart B, Michalski H, Delorme N, Chapparo G, Polu JM. Reliability of six pulse oximeters in chronic obstructive pulmonary disease. Chest 1991; 99: 842-846.
Hansen JE, Casaburi R. Validity of ear oximetry in clinical exercise. Chest 1987; 91(3): 333-337.
Hess DR. Pulse oximetry: Beyond SpO2. Resp Care 2016; 61(12): 1671-1680.
Kohyama T, Moriyama K, Kanai R, Kotani R, Kotani M, Uzawa K, Satoh T, Yorozu T. Accuracy of pulse oximeters in detecting hypoxemia in patients with chronic thromboembolic pulmonary hypertension. PLOS One 2015; 10(5): e0126979
Luks AM, Swenson ER. Pulse oximetry at high altitude. High Altitude Medicine and Biology 2011; 12(2): 109-119.
McGovern JP, Sasse SA, Stansbury DW, Causing LA, Light RW. Comparison of oxygen saturation by pulse oximetry and CO-oximetry during exercise testing in patients with COPD. Chest 1996; 109: 1151-1155.
Nitzan M, Romem A, Koppel R. Pulse Oximetry: fundamentals and technology update. Medical Devices: Evidence and Research 2014; 7: 231–239
Ortiz FO, Aldrich TK, Nagel Rlm Benjamin LJ. Accuracy of pulse oximetry in sickle cell disease. Am J Respir Crit Care Med 1999; 159: 447-451.
Piatkowski A, Ulrich D, Grieb G, Pallua N. A new tool for the early diagnosis of carbon monoxide intoxication. Inhalation Toxicology 2009; 21(13): 1144-1147.
Schnapp LM, Cohen NH. Pulse oximetry. Uses and abuses. Chest 1990; 98(5): 1244-1250.
Tremper KK. Pulse oximetry. Chest 1989; 95(4): 713-715.
Touger M, Bimbaum A, Wang J, Chou K, Pearson D. Performance of the RAD-57 pulse CO-oximeter compared with standard laboratory carboxyhemoglogin measurement. Ann Emerg Med 2010; 56: 382-388.
Weaver LK, Churchill SK, Deru K, Cooney D. False positive rate of carbon monoxide saturation by pulse oximetry of emergency department patients. Resp Care 2013; 58(2): 232-240.
Yamamoto LG, Yamamato JA, Yamamoto JB, Yamamoto BE, Yamamoto PP. Nail polish does not significantly alter oximetry measurement in mildly hypoxic subjects. Resp Care 2008; 53(11): 1470-1474.
Yamiya Y, Bogaard HJ, Wagner PD, Niizeki K, Hoplins SR. Validity of pulse oximetry during maximal exercise in normoxia, hypoxia and hyperoxia. J Appl Physiol 2002; 92: 162-168.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License


Hello, my unseen hero of “all things pulmonary”!
You have helped me SO MUCH in the past….including after a visit to National Jewish Hospital eith a pulmonologist. I was pkeased to learn that their computer models now employ the “LLN” parameters, which showed that althoughmy my FEV1/FVC was at 65%, this fell within a “normal variance” for my age, height (and weight?).
My question (having just read your new post regarding Pulse Ox finger units) is this….I run 4 times a week for 5.5 miles (14 minute mile)….the first thing I do when I finish my run is take my pulse ox and BP.
The pulse ox is ALWAYS between 95-97%…should I trust this reading?….and what are the implications of taking this readings immediately after an intense run? Should I be checking later as well to get a more accurate sense of oxygenation?
…for the millionth time….THANK YOU fir your time and expert advice!
Gregory Price
Gregory –
I think that when you’re referring to your FEV1/FVC ratio it is 0.65, not 65% of predicted. The FEV1/FVC ratio decreases with age, so depending on your age what your pulmonologist told you is probably correct. The issue of what constitutes a normal FEV1/FVC ratio is something that I and the pulmonary physicians I work with have been discussing lately. The ATS/ERS interpretation standards from 2005 advocates the use of the LLN (Lower Limit of Normal) which is statistically derived from the standard deviation of the population being studies and its usefulness depends on the sophistication of the underlying analysis. Without going off too far on a tangent here I’ll say that our current consensus so far is that the LLN probably underestimates airway obstruction in the young and overestimates it in the elderly but this our opinion and doesn’t have a lot of facts to back it up. Having said that all of the thresholds for a normal FEV1/FVC ratio are to one extent or another a line in the sand.
I’m sure that your oximeter reading of 95%-97% is reasonably accurate but that assumes that you don’t have an elevated level of carboxyhemoglobin in your blood (unlikely if you’re not a smoker) or methemoglobin (also unlikely). If you can run 5.5 miles 4 times a week it’s unlikely that you have any problem with gas exchange or oxygenation. Most individuals that desaturate during exercise usually take a little while before their O2 saturation starts to recover after they stop exercising so as long as you take a reading as soon as can after you stop running then it’s probably fine.
– Richard
Good review of the literature, and nice article and post. I agree with all your conclusions. I worked with PhysioControl in the mid ’80’s on validation of their reflection oximeter, a bulky device attached to the ear with headgear. We did various comparisons of abg’s and the readings at various fio2’s, down to 70% as I remember.
Now, at the other end of the table, often being attached to such devices, I sometimes as the MA, RN, whoever, if they know how it works and what it’s limitations are. You can imagine the answers.
Glad you’re still out there, doing the work.
On a recent visit to Swedish in Seattle to see my cardio guy, I ran into the medical director of my lab back in the day. He told me that CPET was more in demand that ever, and the cardio guys were ordering the test. He then asked if I wanted my old job back.
I told him I now lived in Montana, and the chances of me moving back to Seattle, or working again, were dim.
Cheers,
Mike Mulligan