Reports are how patient test results are distributed. Paper versions have become less common because reports are now stored electronically in hospital information systems. Even if the way in which a report’s image is now stored, retrieved and distributed has changed, reports are still generated by our lab’s software systems and the ways in which this is done have not changed in any significant way for quite a while.
Reports are the public face of any pulmonary function lab and they should be designed to be readable and pertinent. It is critically important for any lab to create and manage reports correctly. So why does our lab software make it so hard to do this?
Over the last several months I’ve had the opportunity to compare the reporting systems of the three largest manufacturers of pulmonary function equipment in the US. There are differences of course between each reporting system since each has its own approach towards formatting, editing and printing reports. What they all share however, is a similar underlying model for reports that I call static report pages.
What I mean by static is that the report elements and their position on a report page are determined and fixed in place when the report is formatted. When the report is printed, regardless of whether the results are present or not, the report page does not change. This means that if you format a report to contain spirometry, lung volumes and DLCO, and the only test you perform is spirometry, when you print the report the sections for lung volumes and DLCO will contain no results but they will still appear.
The number of tests that need to be placed on a report will vary from lab to lab depending on what equipment they are equipped with. For example, these tests are available on one manufacturer or another’s test systems:
Spirometry
Lung Volumes – Plethysmography
Lung Volumes – N2 Washout
Lung Volumes – Helium Dilution
Diffusing Capacity
RAW/SGaw
MIP/MEP
MVV
SBN2
6MWT
FOT/IOS
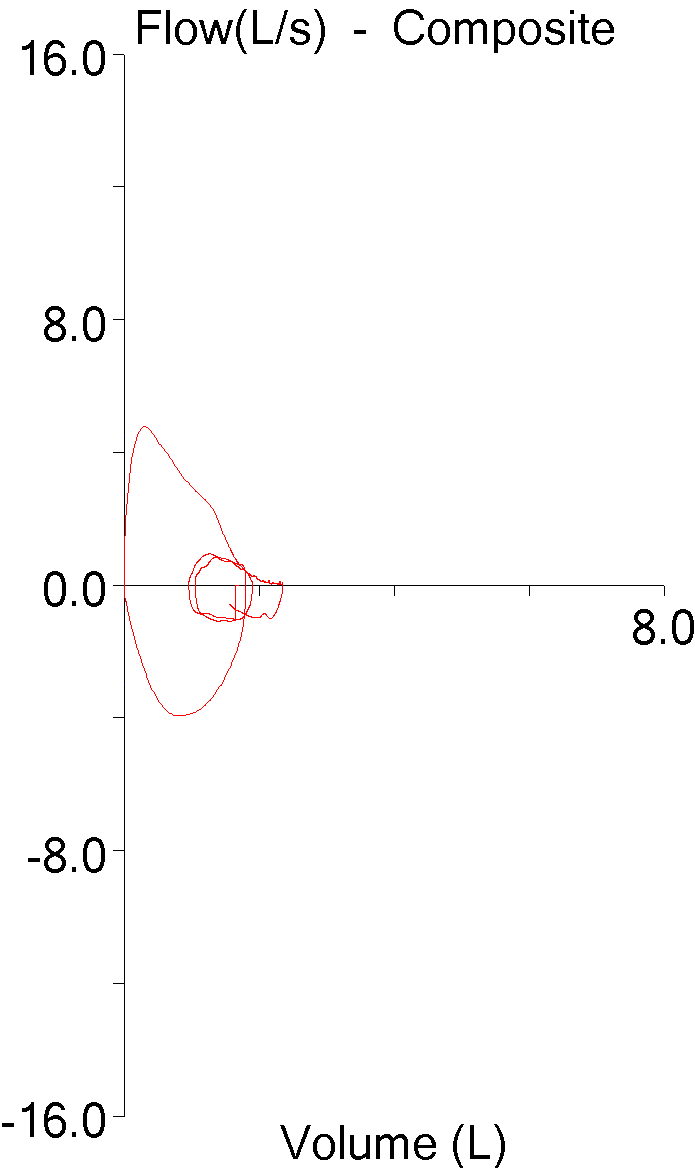
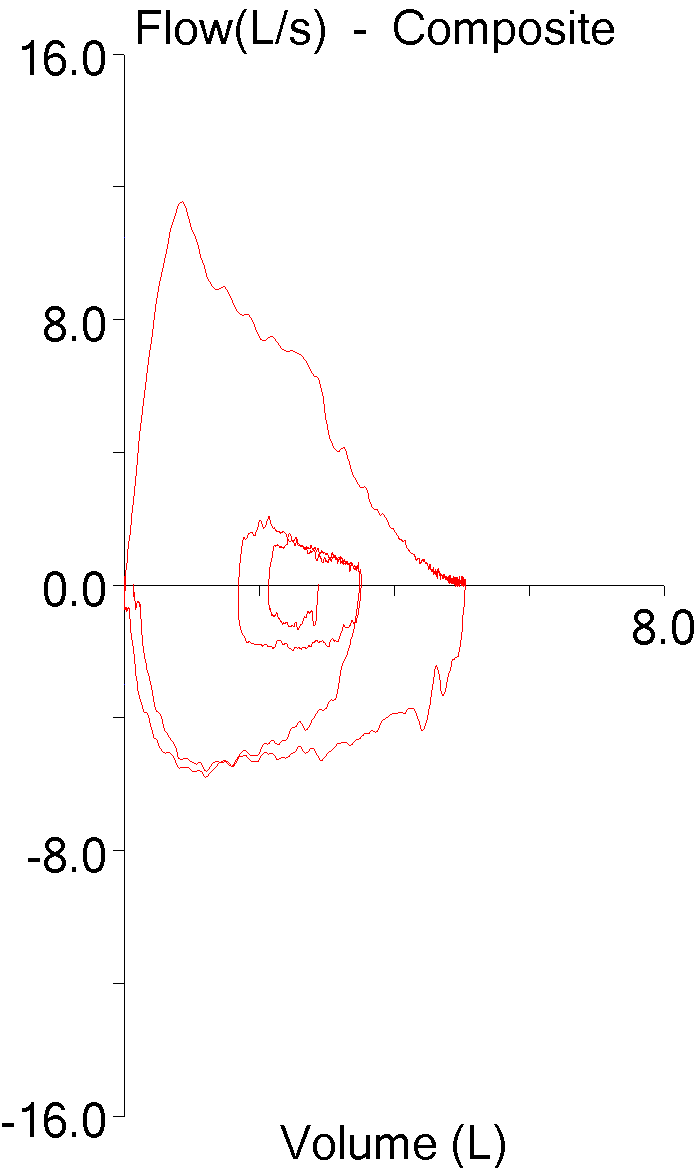
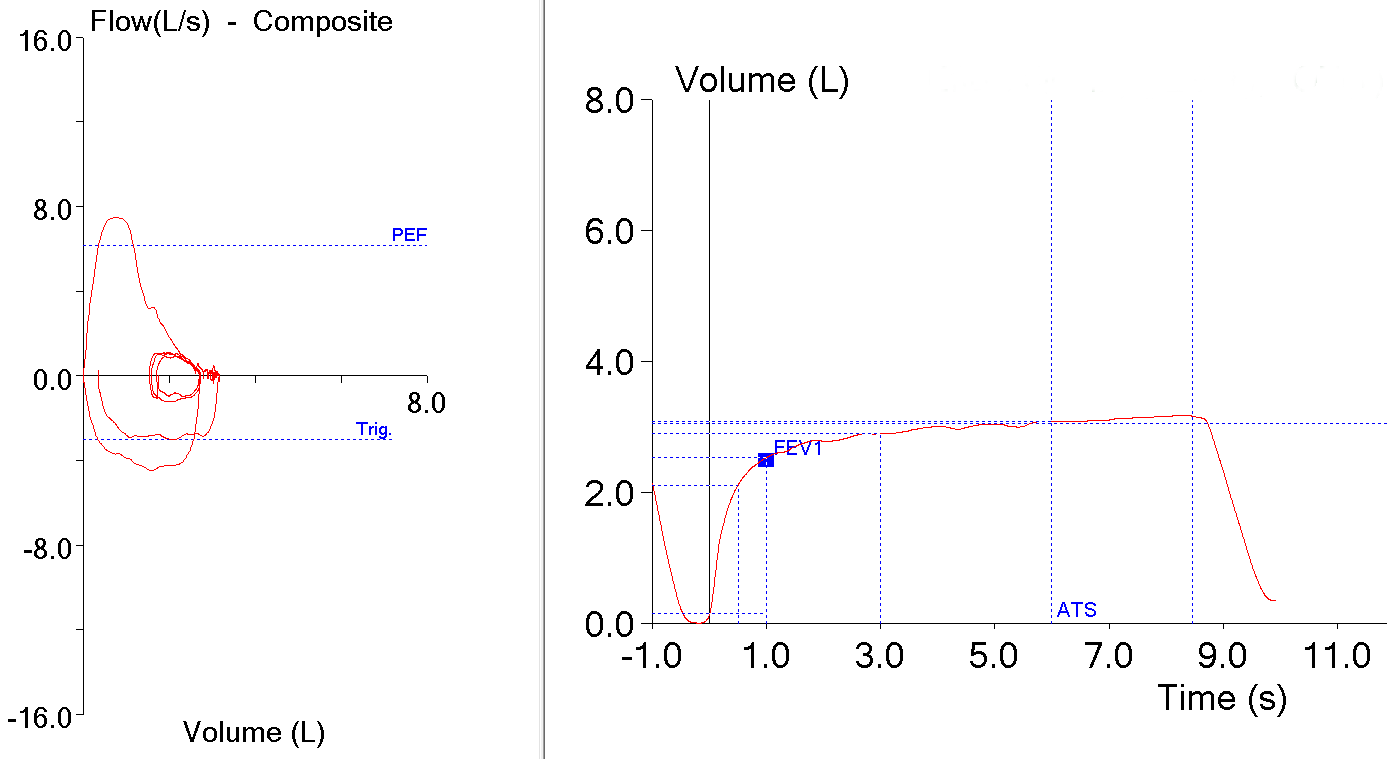
There are probably other tests as well but even if there aren’t, there are other report elements such as demographics, text notes, flow-volume loops, trends etc. that also need to be managed.
Continue reading →