When DLCO tests are performed my lab’s standard policy to average two or more results that meet the criteria for quality and reproducibility. It is not unusual for us to perform three DLCO tests and have all of them meet quality criteria but to have one test result that is higher than the other two. Unlike spirometry tests, bigger isn’t necessarily better for DLCO, so in a circumstance like this we will average the two closest results rather than choose the highest result. Even though the higher test results can come from a DLCO test with good quality, I think that reproducibility trumps this and that choosing by reproducibility gives us results that are more clinically reliable.
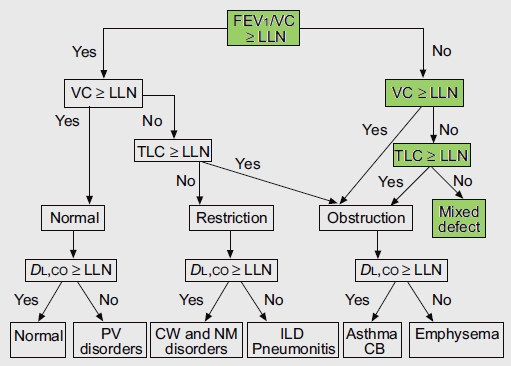
When I review spirometry results and either lung volumes or a DLCO test has also been performed, I will always check the Slow Vital Capacity(SVC) from the lung volumes and the Inspiratory Volume (Vinsp) from the DLCO test to see if they are larger than the reported Forced Vital Capacity. If either of them is I will manually re-calculate the FEV1/VC ratio to see if it indicates the presence of airway obstruction. This is in line with the ATS-ERS recommendations to use the largest Vital Capacity, regardless of the source, for the FEV1/VC ratio.
I have been reviewing the raw test data for all DLCO tests (as well as all the lung volume tests and regular spot checks on spirometry) performed in my lab for at least the last year. Since our software and hardware upgrade a year and a half ago we’ve found a number of problems that have significant effects on the DLCO test results. Depending on the problem they are capable of causing the results to be over- or under-estimated. All of the technicians performing the tests are now well aware of these problems and there haven’t been any problematic DLCO tests selected for a while. Nevertheless, I always check the raw data just to be sure.
Today, I ran across a report that looked quite straightforward. A set of spirometry and DLCO tests had been performed on a frequent-flier patient with pulmonary fibrosis. The patient has restrictive lung disease and lung volumes measured about a year ago were 64% of predicted. Even though the patient’s FVC has decreased since then there is no clinical reason to repeat the lung volume measurements. The results looked like this:
| |
Observed: |
%Predicted: |
Predicted: |
| FVC (L): |
2.28 |
51% |
4.45 |
| FEV1 (L): |
1.64 |
51% |
3.21 |
| FEV1/FVC (%): |
72 |
100% |
72 |
| DLCO ml/min/mmHg: |
12.03 |
50% |
24.23 |
| Vinsp (L): |
2.29 |
|
|
Continue reading →