One of the more significant changes that appeared in the 2017 ERS/ATS DLCO standards was the requirement that rapid-response gas analyzer (RGA) systems calculate VA using a mass balance approach. This is actually more straightforward than it sounds but it does raise several issues that weren’t fully addressed in the 2017 standards.
Up until this time VA has been calculated from the inspired volume and by the amount of dilution of the tracer gas in the exhaled alveolar sample. Specifically:
Which is described by:
Where:
VI = inspired volume
Vd = Anatomical and Machine deadspace
Fitrace = Inspired tracer gas concentration
FAtrace = Exhaled tracer gas concentration
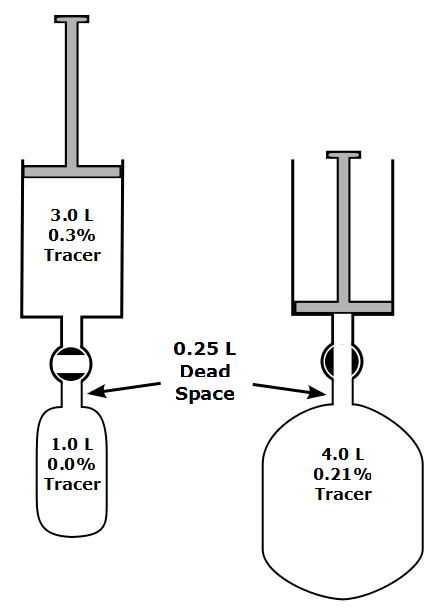
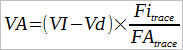
The basic concept behind the mass balance approach to measuring VA is relatively simple and is described in the 2017 standard as:
“…the tracer gas left in the lung at end exhalation is equal to all of the tracer gas inhaled minus the tracer gas exhaled.”
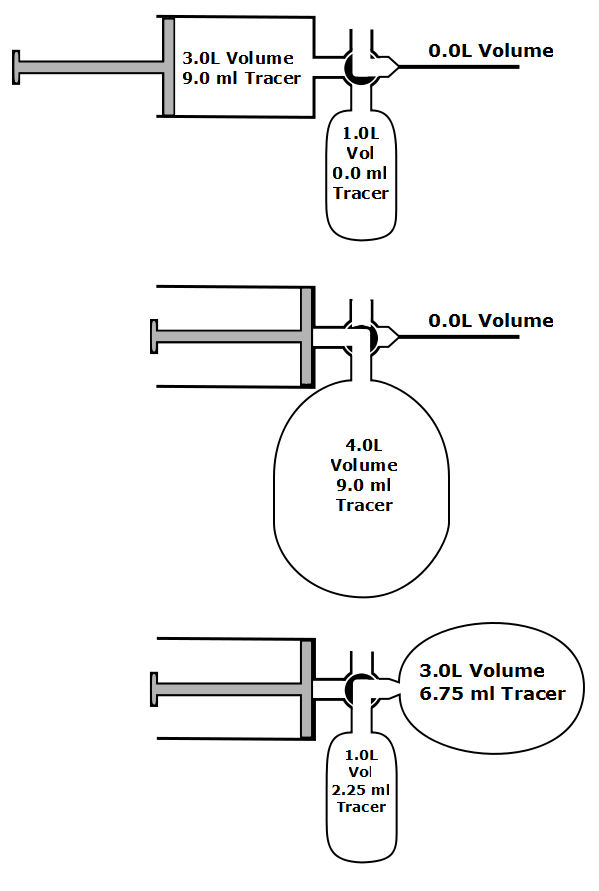
In a flow-based RGA system, after breath-hold the subject exhales to RV and the exhaled volume is integrated from the flow signal. The gas analyzer signal, which is delayed by transit and analyzer response time, is aligned with the flow signal and the exhaled tracer gas volume is integrated from the aligned signals.
End exhalation lung volume (VEE) is calculated using the average of the tracer gas concentration during the last 250 ml of exhaled gas and the volume of tracer gas volume that remains retained in the lung. Alveolar volume is then calculated as:
Note: VdAnatomical is now measured using the Fowler technique rather than being calculated from body weight or height.
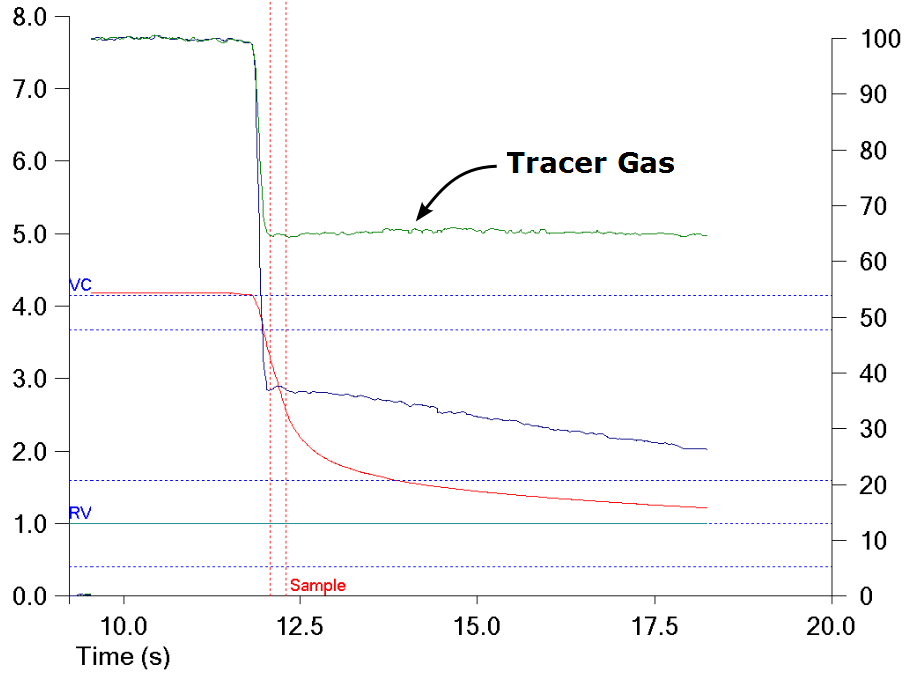
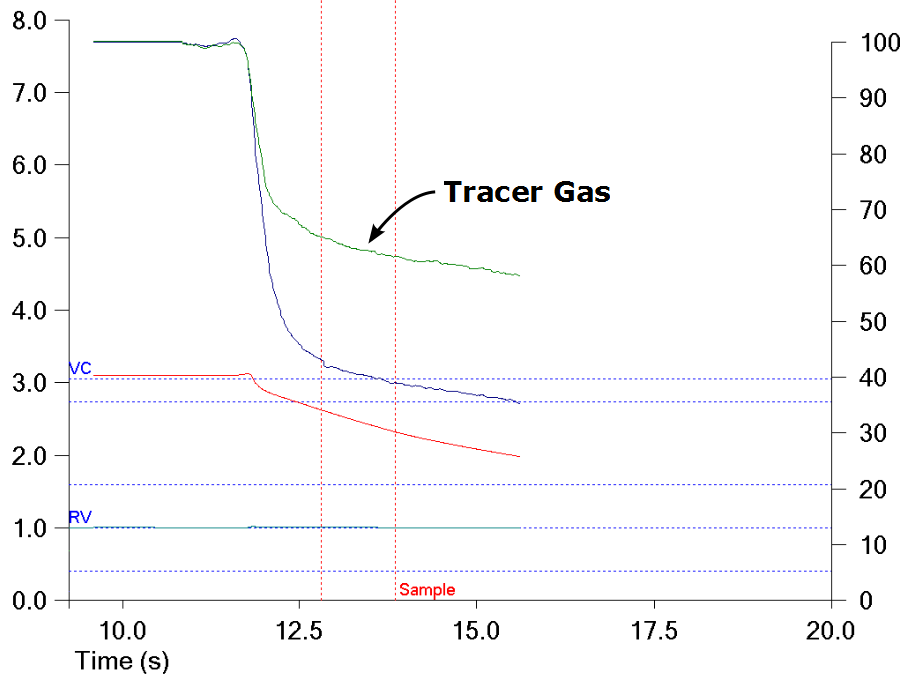
In individuals with normal lungs the DLCO test gas mixture is usually homogenously mixed throughout the lung. When the exhaled DLCO gases are displayed this is usually seen as a flat tracer gas concentration.
For these individuals there will likely be little difference in the VA measured by alveolar sample concentrations and the VA measured by mass balance. In individuals with airway obstruction there is often a significant level of ventilation inhomogeneity. When this occurs it is usually seen as a sloping tracer gas line.
For these individuals the VA measured by mass balance will be higher than the VA measured by dilution. Since the way in which the CO concentration is measured (i.e. an alveolar sample) has not changed, this will lead to a higher value for DLCO. This is mentioned in the 2017 standards where they indicate that:
“The resulting DLCO measurements in COPD cases are some 8 to 15% higher.”
The standard also notes that ventilation inhomogeneity also occurs as part of aging that elderly individuals with normal lungs may also have a higher DLCO when VA is calculated by mass balance. Although not directly stated as such the 2017 standard implied that the normal DLCO reference values for elderly individuals may no longer be representative and that new studies will be required for all age groups.
The justification for calculating VA by mass balance is that it leads to a VA that will more closely approximates an individual’s actual TLC and that reproducibility will be improved. DLCO is calculated however, using the average CO concentration from the alveolar sample, not from the entire exhalation, and this makes the assumption that the CO uptake within the rest of the lung will be the same. Although this is likely to be reasonably true in individuals with normal lungs, it’s not clear how well this applies to patients with lung diseases.
One of the studies cited for the mass balance calculation of VA, Horstman et al, showed a series of graphs of DLCO/VA versus lung volume for subjects with normal lungs and subjects with COPD. The graphs for the normal subject showed a slight increase in DLCO/VA at exhaled volumes beyond the alveolar volume, whereas COPD patients showed a slight decrease. This at least implies that DLCO is homogeneous enough for the alveolar CO sample to be reasonably representative. The most notable finding however, was that the increase in DLCO seen in COPD patients was almost exactly proportional to the increase in VA measured by the mass balance approach.
Note: DLCO/VA (aka KCO, which is not the diffusing capacity per liter of alveolar volume despite being stated as such in the article) normally rises when measured at at lung volumes below TLC but in this study DLCO/VA (KCO) was measured at intervals during exhalation from an inhalation that was to TLC.
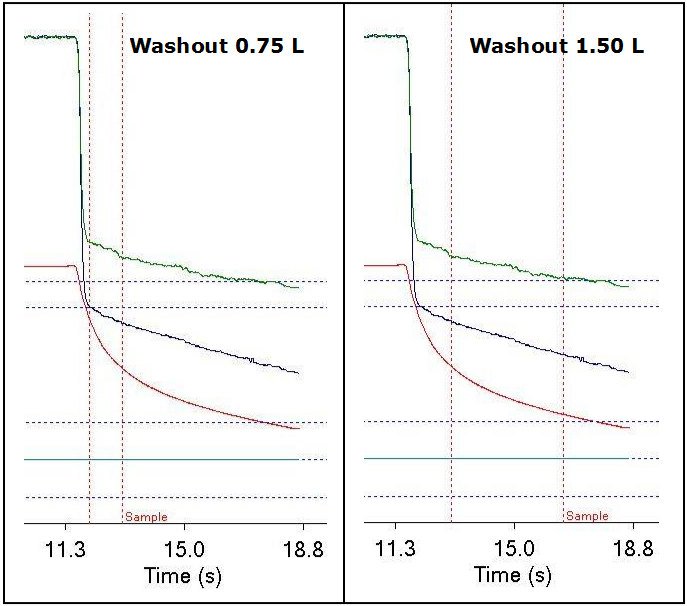
Some experimentation by myself along vaguely similar lines showed that changing the DLCO washout volume for a patient with very severe COPD (FEV1 33% of predicted) actually made little difference in DLCO:
| Washout 0.75 L | Washout 1.50 L | |
| DLCO: | 10.75 | 10.84 |
| VA: | 4.95 | 5.31 |
| BHT: | 10.86 | 13.11 |
Despite all this I have several issues that are not exactly objections, but are at least significant questions about the change in the way VA is calculated.
First, there is a conceptual issue. The VA measured by dilution has been characterized as the lung volume “seen” by the DLCO test while the VA measured by mass balance could be said to contain some “hidden” lung volume. This is not the first time that VA has been measured by indirect methods. In fact the original paper by Ogilvie et al in 1957, which set the standards for the single-breath DLCO, found that when VA was compared to TLC that the result was:
“…useless in all but extreme circumstances”
And recommended that VA be calculated in in a two-step process. Specifically, RV was measured either by helium dilution or N2 washout and VA was then calculated from:
VA = VI + RV
This approach towards measuring VA was criticized relatively quickly, partly because of the extra time required for the process but also because it was generally decided that VA measured by dilution was the “effective volume” and that adjusting VA to TLC was an inappropriate extrapolation. The method of calculating VA from VI and RV was sidelined and has been rarely used since that time.
Any difference in DLCO between the two techniques is primarily related to the difference in VA volumes. So is DLCO is more correct when calculated with the “effective” volume determined by dilution or when VA is measured by mass balance? I think this is a valid question because the mass balance VA is measured using the tracer gas concentration from the entire exhalation while exhaled CO is still measured using a standard alveolar sample. The answer has to be whether the extra volume participates in the same level of gas exchange as the rest of the lung and I can see arguments both for and against this point.
Realistically however, the same question can be applied to the DLCO calculated with an “effective” volume where a small alveolar sample is used to represent the entire lung. Since Horstman et al measured DLCO using most of the exhaled CO concentration instead of just an alveolar sample this question could have been avoided and overall DLCO accuracy improved (at least potentially) if this had been included in the 2017 standard, but since this option was not discussed it’s not possible to say why it wasn’t considered.
Next, the mass balance VA requires an accurate alignment of flow and gas analyzer signals. Although the 2017 standards specify the analyzer response time there were no specifications for sample transit time (lag time) nor were there recommendations about how it should be measured. In addition the possible error from misaligned signals has not been characterized. I bring this up because the transit time calibration on my lab’s DLCO systems routinely changes by between 20 and 40 milliseconds from one calibration to another, even when they are performed back to back. A small misalignment in signals probably won’t reduce accuracy by all that much, but at the moment it’s hard to say what actually constitutes a small misalignment and what constitutes a significant one.
Finally, the CH4 concentration near the end of exhalation is used to calculate the VEE and this assumes that the tracer gas concentration is homogeneously distributed through this volume. The CH4 curve from a patient with COPD however, shows a steady decrease in tracer gas throughout exhalation and if this is extrapolated it implies that the CH4 concentration within the VEE is less than that it is at end-exhalation. This in turn implies that under these circumstances the VEE is being underestimated.
Moreover, the accuracy of the VEE and mass balance VA is to some extent dependent on a full exhalation to RV following the breath-hold. The 2017 standards however, do not include any quality indicators for exhalation past acquiring the alveolar sample. It’s unclear what effect a suboptimal exhalation will have on VEE and the mass balance VA.
The changes involved in the 2017 DLCO standards will provide the fodder for any number of technical and clinical research studies. The biggest changes in DLCO will likely be seen in lung disorders with some degree of ventilation inhomogeneity but since it has not been studied across the full range of obstructive and restrictive lung disorders it’s not possible to predict where differences in DLCO may appear. In particular, because ventilation inhomogeneity normally increases with age, new reference equations will be needed sooner rather than later.
I have no significant objections towards measuring VA by mass balance. It’s relatively straightforward and at least as valid an approach as measuring VA by dilution. Since it requires the proper operation of a number of mechanical, electronic and software systems I will however, retain some reservations about the accuracy of this approach until some of the possible errors are better characterized.
The new 2017 standards do not make “classical” DLCO systems obsolete and most labs are unlikely to be able to implement its recommendations on VA immediately. Many of us will have to wait until our current testing systems are replaced before having to deal with the new aspects of the 2017 standards, and capital budgets being what they are, that is probably years away. Although my lab’s equipment already have RGAs, we will need a fairly significant software update before we measure VA by mass balance and since our equipment vendor is not particularly noted for the rapidity at which it updates its software I suspect we will also have a prolonged wait.
What the new standard does is to provide a road map for the future. At some point we will have to deal with the fact that some patients will have noticeable change in their DLCO. Given that for most of us this will be a while in the future, there will probably be time for at least some of the technical and clinical research to catch up before we have to take that step.
References:
Graham BL, et al. 2017 ERS/ATS standards for the single-breath carbon monoxide uptake in the lung. Eur Respir J 2017; 49: 1600016.
Horstman MJM, Health B, Mertens FW, Schotborg D, Hoogsteden HC, Stam H. Comparison of total-breath and single-breath diffusing capacity in healthy volunteers and COPD patients. Chest 2007; 131: 237-244.
Mortin JW, Osborne LG. A clinical review of the single breath method of measuring the diffusing capacity of the lungs. Chest 1965; 48: 44-54.
Ogilvie CM, Forster RE, Blakemore WS, Morton JW. A standardized breath holding technique for the clinical measurement of the diffusing capacity of the lung for carbon monoxide. J Clin Invest 1957; 36: 1-17.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License

Hello Richard,
I discovered your blog yesterday. Congratulations on a very informative resource.
As I recall, I did my first DLCO measurement at the Georgetown University Hospital in 1966 using a gas chromatograph. I stayed in the pulmonary function field until 1997 then went into industry. Now I’m considering getting back, and would like to investigate some of the new technology. Can you give me any details on the rapid gas analyzer you are using for DLCO measurements ?
Thank you,
Lou Wilkinson
Lou –
I’ve never been able to find a technical description of the rapid gas analyzer. I was told by a service tech that there is a rotating filter wheel that selects for specific wavelengths of infrared and near-infrared that corresponds to the absorption spectrum of CO and CH4. It (allegedly) rotates at 1000 hz but whether this is the sampling frequency for one wavelength or for all 5 (i.e. 200 hz for a single channel) I don’t know. I’ve also been told (again can’t verify) that the signal to noise ratio is on the low side so that a fair amount of software correction is needed.
On the plus side, you can select the alveolar plateau after the test has been performed so you don’t have to preset a washout and sample volume and get stuck with whatever you get. On the minus side, I have some concerns about how well the gas signals are matched with the flow signal (they occur at different times because the gas signal is delayed by sample transport and analyzer rise-fall time) since this has a direct bearing on the measured volume of CO and CH4. I can say from my own experience that my lab’s test systems seem to be sensitive to exhaled flow rates because a slow exhalation usually has a low dead space and a fast exhalation usually has an elevated dead space.
I will also mention that the difference in DLCO measured by discrete sampling systems (the old alveolar bag approach) has never been systematically compared to the DLCO measured by rapid gas analyzers. Theoretically a rapid gas analyzer system should be more accurate but I have concerns about how well this technology is actually implemented and of note, the average DLCO measured in population studies has decreased by at least 10% since rapid gas analyzers came into common use.
Regards, Richard
Richard, thank you for your rapid reply !
Given the competitive nature of commercial PFT systems it’s not surprising that manufacturers do not give complete details about their analyzers. Furthermore, most technicians would not be interested, since these details would add little to their ability to do quality testing. For old timers such as myself, who started measuring oxygen saturation with the Van Slyke machine, not having a complete understanding of the instrumentation we use is a bit disturbing. Almost everything today is done with software, and becomes more automated with each passing year. The same is true in the industrial field where robots are rapidly replacing skilled workers.
Oh well – so much for the rambling of a dinosaur. I’ll go over to the Cal State Fresno library and see what I can dig up about NDIR analyzers. Maybe I can make one :).
Best regards,
Lou