The Maximum Voluntary Ventilation (MVV) test was initially described in 1933. It was the first pulmonary function test that involved inspiratory and expiratory air flow in a significant way and for this reason it helped to set the stage both conceptually and technically for the FEV1, the FEV1/FVC ratio and our present understanding of obstructive lung diseases. MVV is reduced in a variety of conditions, including obstructive, restrictive and neuromuscular diseases, but a reduced MVV is non-specific and this limits its clinical utility. Nevertheless, it continues to be performed both in clinical labs and for research, and for this reason it would seem to be a good idea to know how to assess MVV results.
As usual, there are two aspects to assessing pulmonary function results; test performance and normal values.
Currently the ATS/ERS statement on spirometry contains the only available standard for performing the MVV test. Unfortunately this standard also contains some significant flaws. Its primary recommendation is that the MVV test be performed with a tidal volume that is approximately 50% of the forced vital capacity and a breathing frequency of around 90 breaths per minute. These recommended values are problematic and some simple mathematics will show why.
A respiratory rate of 90 BPM means that there is 2/3 of a second for both inhalation and exhalation. With a 1:1 ratio for inspiration and expiration, there is only 1/3 of a second for exhalation. Since it normally takes a full second to exhale approximately 75% of the vital capacity (i.e. the FEV1), 1/3 of a second would only allow time to exhale 25% of the vital capacity (not exactly true of course, but it helps prove the point). How then is it possible to exhale 50% of the vital capacity, twice that amount, in the same amount of time? The answer is that it isn’t and if it was somehow possible for somebody to actually meet the ATS/ERS recommended values they would have an MVV that would be 45% to 100% higher than any of the predicted MVV’s. I suspect the ATS/ERS agrees this is a problem since following the initial recommendation it also says that “… since there are little data on MVV acceptability criteria, no specific breathing frequency or volume is required”.
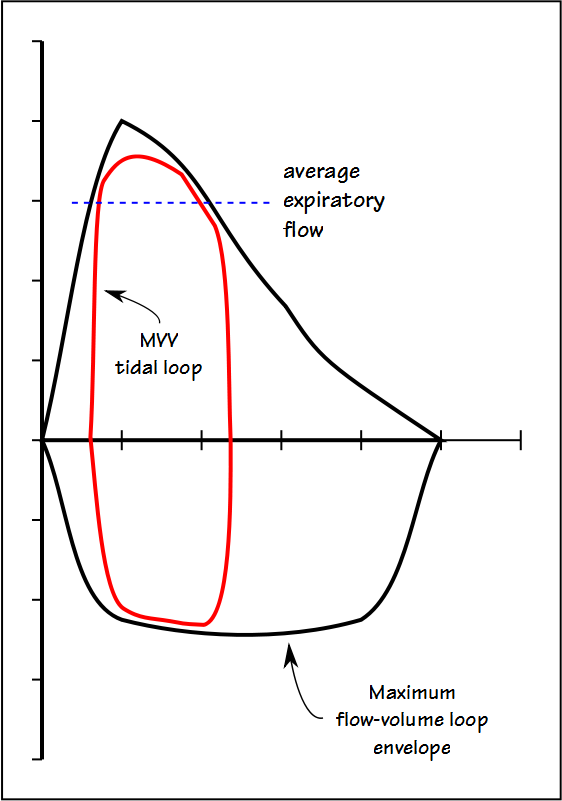
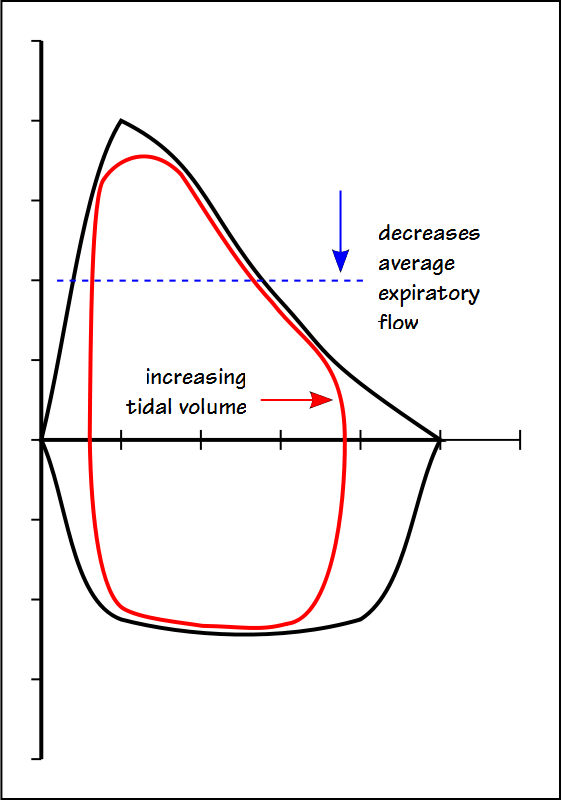
The fact is that no single tidal volume recommendation is going to work for all patients and this is because the MVV tidal volume has to reside mostly within the maximal flow-volume loop envelope.
This means that increasing the MVV tidal volume comes at the expense of decreasing the average expiratory flow rate, which in turn will decrease the MVV.
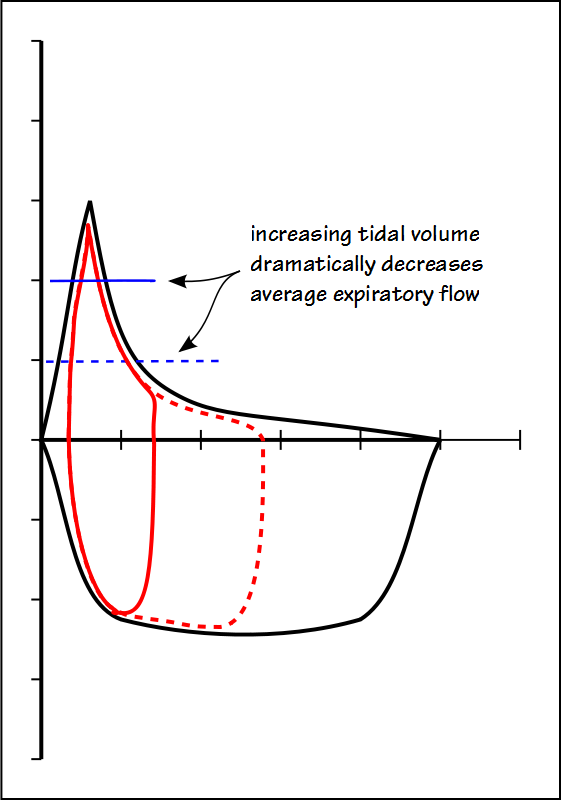
In individuals with normal lungs, there is still a fairly broad range of lung volumes where the average expiratory flow rate is relatively high. When obstructive disease is present however, there is only a narrow range of lung volumes where high expiratory flow rates are possible and any attempt to increase tidal volume will dramatically decrease the average expiratory flow rate.
This means that a tidal volume anywhere near 50% of the vital capacity is probably going to be counterproductive in individuals with airway obstruction.
It’s not clear that a respiratory rate of 90 is correct either, since at least one study has indicated that MVV tends to decrease at respiratory rates above 80. In addition, since one of the primary clinical reasons to perform an MVV test is to assess an individual’s maximum ventilatory capacity for an exercise test and an exercise respiratory rate above 55 is considered abnormal. Having said that, MVV ventilation is not the same as exercise ventilation and they should not be considered equivalent.
I think that the final answer is that each individual is going to have their own optimum tidal volume and respiratory rate. The overall quality of an MVV should be judged first by multiplying an individual’s FEV1 x 40. The ATS/ERS standard says that an MVV less than 80% of this value is likely suboptimal. If a test result does not meet this criteria then subjects should be corrected if their respiratory rate is too high (greater than 90?) or too low (less than 60?), or if their tidal volume is too large (greater than 50% of VC?) or too small (less than 25% of VC?).
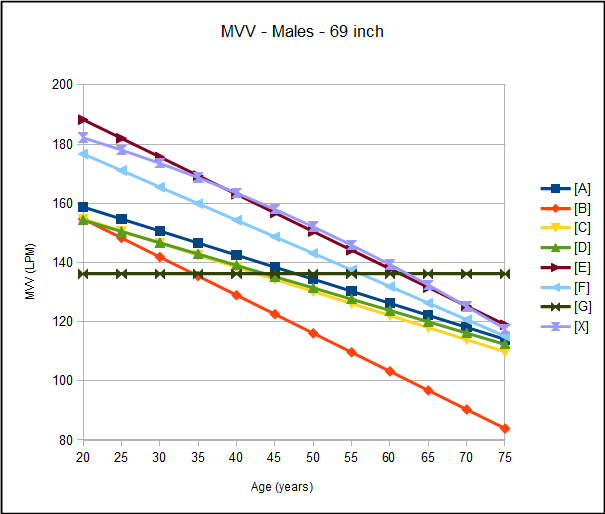
Compared to most other spirometric parameters there are relatively few reference equations for MVV. This number is even more limited by the need to exclude MVV population studies prior to the 1960’s. Relatively early in the study of MVV there was some appreciation of equipment resistance and inertia but it was not until the 1960’s that testing systems able to routinely produce accurate MVV results came into common use.
As usual there are always problems associated with selecting a specific reference equation. Several of the reference equations, particularly those for females, are quite limited because only a single factor, either age or height, is used to calculate the predicted MVV and for this reason these reference equations should be avoided. Most of the studies have a limited population size with a limited range of ethnicities. This makes it unclear what effect, if any, ethnicity has on predicted MVV.
More than one study however, has shown there is a strong relationship between FEV1 and MVV. Depending on the study FEV1 can be multiplied by 35, 37.5 or 40 to obtain the predicted MVV. Since FEV1 is an expiratory measurement, any limitations to inspiratory flow will affect MVV as well, but inspiratory airway obstruction is relatively rare. Because the reference equations for FEV1 are well characterized by age, sex and ethnicity I think it is probably best to use FEV1 to derive the predicted MVV, particularly given the limitations of the existing MVV population studies. Since the ATS/ERS uses FEV1 x 40 to judge the adequacy of the MVV test then it would also seem best to use predicted FEV1 x 40 to derive predicted MVV as well.
I still have significant reservations about the utility of the MVV test. Because it is reduced in many different lung diseases it has little specificity and for this reason its clinical utility is limited. In addition I think that it is a stressful test for patients with poor lung function but even individuals with normal lung function can have difficulty performing the test correctly. The most common uses of the MVV test are as a pre-exercise assessment and as a general indication of lung health. For these reasons the MVV test continues to be performed so those performing it need to have a reasonable idea how it should be assessed.
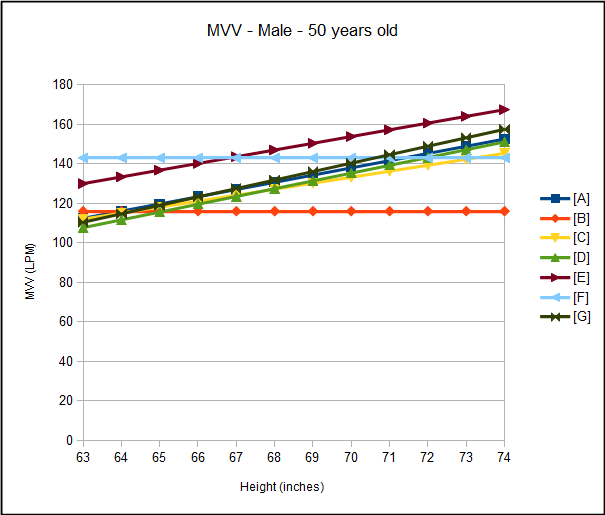
Male MVV Reference Equations
| Study: | No: | Age Range: | Equation: |
| [A] | 247 M+F | 21-75 | (3.65 x ht(in)) – (0.814 x age) – 76.78 |
| [B] | 62 | 20-65 | 180.5 – (0.1288 x age) |
| [C] | 879 | 15-79 | (3.02915 x ht(in)) – (0.81621 x age) – 37.94893 |
| [D] | 270 | 20-70 | (3.943 x ht (in)) – (0.7629 x age) – 102.5 |
| [E] | 468 | 20-65 | (3.404 x ht(in)) – (1.26 x age) – 21.4 |
| [F] | 50 | 20-80 | 199.1 – (1.12 x age) |
| [G] | 130 | 17-78 | (4.2776 x ht(in)) – 159.01 |
| [X] | NHANESIII FEV1 x 40 |
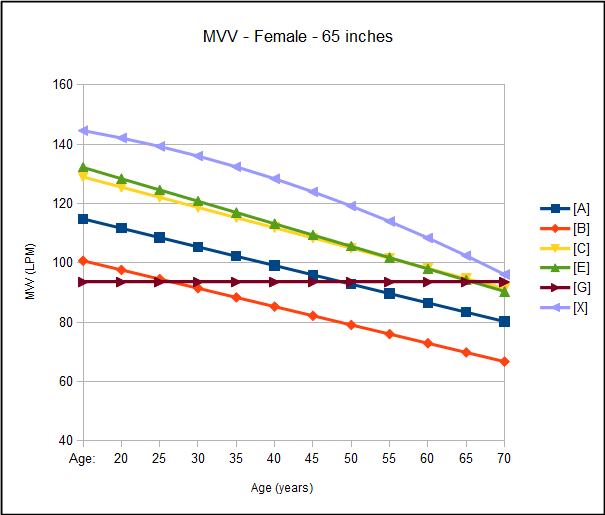
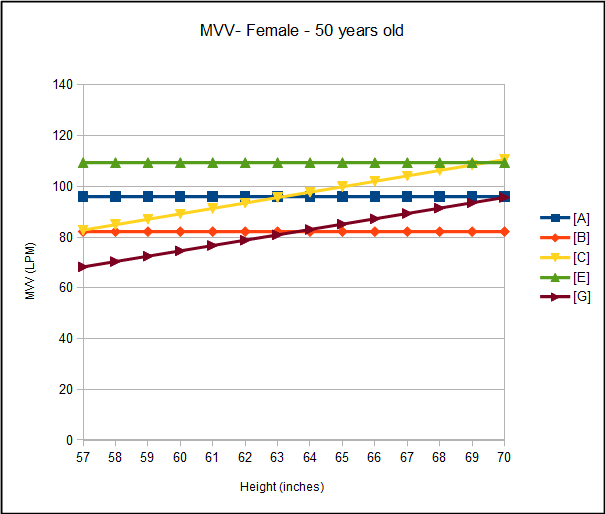
Female MVV Reference Equations:
| Study: | No: | Age Range: | |
| [A] | 247 M+F | 21-75 | 127.43 – (0.629 x age) |
| [B] | 58 | 20-65 | 113.1 – (0.618 x age) |
| [C] | 452 | 15-79 | (2.13844 x ht(in)) – (0.68503 x age) – 4.86957 |
| [E] | 50 | 20-80 | 147.4 – (0.76 x age) |
| [G] | 153 | 16-68 | (2.106 x ht(in)) – 51.7555 |
| [X] | NHANESIII FEV1 x 40 |
References:
Bartlett RG, Phillips NE, Wolski G. Maximum voluntary ventilation prediction from the velocity-volume loop. Chest 1963; 43: 382-392.
[A] Bass H. The flow volume loop: Normal standards and abnormalities in chronic obstructive pulmonary disease. Chest 1973; 63: 171
[B] Birath G, Kjellmer I, Sandqvist L. Spirometric studies in normal subjects. Part II. Ventilatory capacity in adults. Acta Med Scand 1963; 173: 193.
Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standardisation of lung function testing. Standardisation of Spirometry. Eur Respir J 2005; 26: 319-338.
Campbell SC. A comparison of the maximum voluntary ventilation with the forced expiratory volume in one second: an assessment of subject cooperation. J Occup Med 1982; 24: 531-533.
[C] Cherniak RM, Raber MB. Normal standards for ventilatgoryfunction using an automated wedge spirometer. Am Rev Resp Dis 1972; 106: 38
Dillard TA, Hnatiuk OW, McCumber TR. Maximum voluntary ventilation. Spirometric determinants in chronic obstructive pulmonary disease patients and normal subjects. Amer Rev Resp Dis 1993; 147: 870-874.
[X] Hankinson JL, Odencrantz JR, Fedan, KB. Spirometric reference values from a sample of the general U.S. Population. Amer J Resp Crit Care 1999; 159: 179-187
Harber P, SooHoo K, Tashkin DP. Is the MVV:FEV1 ratio useful for assessing spiromtry validity? Chest 1985; 88: 52-57.
[D] Hedenstrom H, Malmberg P, Fridrikkson HV. Reference values for lung function tests in men: regression equations with smoking variable. Upsala J Med Sci 1986; 91: 299-310
[E] Kory RC, Callahan R, Boren HG, Syner JC. The Veterans Administration-Army cooperative study of pulmonary function. Part I. Clinical spirometry in normal men. Am J Med 1961; 30: 243
[F] Neder JA, Andreoni S, Lerario MC, Nery LE. Reference values for lung function tests. II. Maximal respiratory pressures and voluntary ventilation. Braz J Med Biol Research 1999; 32: 719-727
[G] Roa CC, et al. Normal standards for ventilatory function tests in adult Filipinos. Phillipine J Int Med 2013; 51(1): 1-6.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.