We have a number of patients who have spirometry and DLCO testing performed at regular intervals. I’ve noticed that every so often DLCO results change significantly without a change in spirometry (or lung volumes) or there’s a modest change in spirometry and a marked change in DLCO. I’ve been concerned that this may be a symptom of problems with our DLCO (CO/CH4) gas analyzers and at least once recently this kind of discrepancy did lead to having an analyzer being serviced. Realistically though, the gas analyzers are routinely passing their calibrations and when I look at the trends in calibration there hasn’t been any systematic drift. This doesn’t rule out intermittent problems however, so in order to find out whether these changes in DLCO are “real” or an artifact of our testing systems I decided to see if taking a closer look at the results would help resolve this.
First, what constitutes a significant change in DLCO?
My lab’s current working definition is an increase or decrease in DLCO that is ≥2.0 ml/min/mmHg or ≥10%, whichever is greater. This is slightly different from the ATS/ERS DLCO intra-session repeatability requirements (≥3.0 ml/min/mmHg or ≥10%) and may mean that we’re setting the bar too low but there’s a difference between intra-session and inter-session variability. Specifically, we average the two closest results (assuming there are at least two tests of good quality) from one testing session to another and it is the inter-session average we are comparing, not individual tests and for this reason we feel that a smaller change can be relevant.
Note: The ATS/ERS statement on interpretation does discuss inter-session DLCO variability but there it is expressed as >7% within the same day and >10% year to year without setting an upper limit. The year to year value is based solely on a study from 1989 on eight individuals using a manually operated testing system (Collins Modular Lung Analyzer) that used a semi-automated alveolar sampling bag and for this reason it’s hard to be sure it is still relevant.
Second, which test parameters have the greatest effect on calculated DLCO?
As a reminder, the DLCO formula is:
Where:
VA = alveolar volume (in ml)
BHT = breath-holding time (in seconds)
Pb = barometric pressure (in mmHg)
FITrace = inspired concentration of the tracer gas (helium, methane, neon)
FATrace = exhaled (alveolar) concentration of the tracer gas
FICO = inspired concentration of Carbon Monoxide
FACO = exhaled (alveolar) concentration of Carbon Monoxide
And:
Where:
Deadspace volume = machine deadspace + anatomic deadspace
In these two formulas FITrace, FICO, PH2O and Deadspace volume are essentially constants and do not change from session to session. Pb may change slightly but its effect is insignificant and can be ignored. Of the remaining parameters FACO will of course have a direct bearing on DLCO, but any changes in BHT tends to cancel themselves out and this is because a longer BHT usually leads to a lower FACO and a shorter BHT leads to a higher FACO. DLCO is therefore going to depend most strongly on FACO, VA, Inspired Volume (VI) and FATrace and less so on BHT. VA, VI and BHT are primarily patient performance issues, while FACO and FATrace are gas analyzer issues.
Note: Hemoglobin also has a significant effect, but I selected only DLCO tests that had been corrected for hemoglobin for this analysis.
So what do these changes look like?
| Session 1: | %Predicted: | Session 2: | %Predicted: | |
| FVC: | 2.69 | 102% | 2.60 | 99% |
| FEV1: | 2.06 | 104% | 1.97 | 100% |
| FEV1/FVC: | 76% | 102% | 76% | 101% |
| DLCO: | 15.18 | 91% | 13.01 | 78% |
| VA: | 4.01 | 88% | 3.88 | 85% |
| VI: | 2.71 | 2.63 | ||
| FACH4: | 59.32 | 60.74 | ||
| FACO: | 33.28 | 36.87 | ||
| BHT: | 10.63 | 10.43 |
Both sessions have DLCO tests that meet the ATS/ERS standards for quality and repeatability. The difference in FVC, FEV1, VA, VI, BHT and FACH4 are minimal. The primary difference is in FACO with about a 10% decrease in CO uptake in the second session when compared to the first. Since there doesn’t seem to be any performance or gas analyzer issues this change in DLCO is likely real.
| Session 1: | %Predicted: | Session 2: | %Predicted: | |
| FVC: | 2.93 | 63% | 3.10 | 67% |
| FEV1: | 2.34 | 67% | 2.35 | 68% |
| FEV1/FVC: | 80% | 107% | 76% | 101% |
| DLCO: | 15.16 | 58% | 18.30 | 70% |
| VA: | 4.19 | 60% | 4.18 | 60% |
| VI: | 3.27 | 2.97 | ||
| FACH4: | 69.84 | 62.21 | ||
| FACO: | 40.15 | 31.81 | ||
| BHT: | 10.63 | 10.66 |
Although there are minimal changes in spirometry values there was a test performance difference with about a 10% decrease in VI in the second session. Interestingly, the VA is the same between both sessions which implies a similar degree of expansion and gas mixing within the lung. What’s suspicious about these tests is that both the FACH4 and the FACO are lower than in the first session and that in an absolute sense the decrease in FACH4 and FACO are similar (-7.63 vs -8.34).
A similar change in absolute values is something you would expect if there had been a shift in the analyzer’s zero or span. Our tests systems perform a zero and span check before every test and when I checked I found them both to be within normal limits for both sessions. Despite this, this one remains suspicious to me.
| Session 1: | %Predicted: | Session 2: | %Predicted: | |
| FVC: | 3.11 | 68% | 3.03 | 67% |
| FEV1: | 2.63 | 70% | 2.57 | 69% |
| FEV1/FVC: | 84% | 101% | 85% | 102% |
| DLCO: | 17.19 | 73% | 15.01 | 63% |
| VA: | 4.01 | 65% | 3.63 | 59% |
| VI: | 3.15 | 2.96 | ||
| FACH4: | 67.35 | 67.91 | ||
| FACO: | 35.34 | 36.76 | ||
| BHT: | 10.47 | 10.33 |
Again minimal changes in spirometry and although there were minimal differences in FATrace and FACO the VI was slightly (-6%) less in the second session. There was a more significant decrease in VA however (-9%) and in fact this alone was likely the major cause of the difference in DLCO between the two sessions.
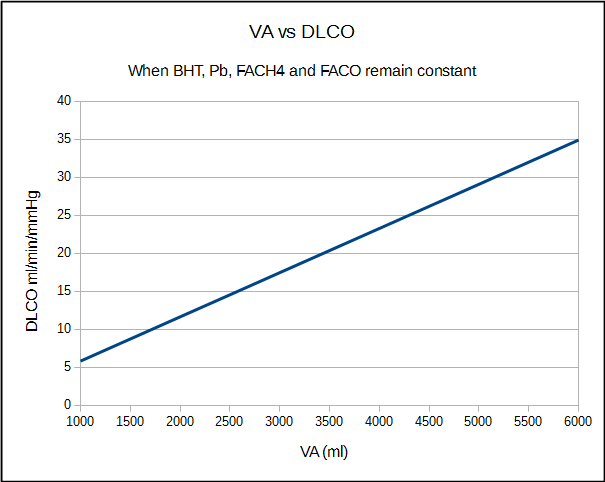
Assuming all other values remain the same DLCO scales linearly with VA.
There were only small differences in most parameters between the two sessions but the difference in DLCO was 2.18 ml/min/mmHg (-13%) and this seems to be due to a decrease in VA of -9% and a decrease in FACO of -4%.
So in this particular case even though the DLCO tests in both test sessions met all ATS/ERS criteria for acceptability, there were performance issues that are likely responsible for most of the difference in DLCO and only small changes in CO uptake that are responsible for the rest.
| Session 1: | %Predicted: | Session 2: | %Predicted: | |
| FVC: | 2.39 | 56% | 2.90 | 69% |
| FEV1: | 1.81 | 56% | 2.07 | 65% |
| FEV1/FVC: | 76% | 100% | 71% | 95% |
| DLCO: | 22.26 | 86% | 16.54 | 64% |
| VA: | 4.12 | 64% | 4.45 | 69% |
| VI: | 2.56 | 2.85 | ||
| FACH4: | 51.67 | 56.60 | ||
| FACO: | 21.77 | 32.06 | ||
| BHT: | 10.88 | 10.62 |
There were significant improvements in spirometry from the first to the second session yet despite this the DLCO decreased by 27%. It could be argued that even though the FEV1 increased the decrease in the FEV1/FVC ratio indicates that airway obstruction was actually slightly more severe but the FEV1/VI ratio from the first session was also 71% so there really was no change. Both sets of DLCO tests met the ATS/ERS criteria for acceptability and reproducibility.
The biggest difference between the two sessions is the FACO and this implies that CO uptake was markedly better in the first session than the second. I could argue that the FACO from that session is too low but given the minimal differences in VA and the fact that there was no systematic difference in FACH4 and FACO I’m going to reluctantly say this is more likely due to changes in the patient’s clinical status.
| Session 1: | %Predicted: | Session 2: | %Predicted: | |
| FVC: | 4.00 | 93% | 4.22 | 98% |
| FEV1: | 2.47 | 78% | 1.95 | 61% |
| FEV1/FVC: | 62% | 84% | 46% | 63% |
| DLCO: | 11.84 | 47% | 5.88 | 24% |
| VA: | 5.44 | 81% | 5.15 | 77% |
| VI: | 2.44 | 4.09 | ||
| FACH4: | 39.45 | 72.83 | ||
| FACO: | 31.14 | 62.15 | ||
| BHT: | 8.94 | 10.71 |
The FEV1 decreased significantly in the second session but the DLCO decreased much more. This however may be comparing apples to oranges. The first session did not meet the ATS/ERS standards for quality or reproducibility (only one vaguely acceptable test was performed) and the VI is quite low compared to the FVC.
What this likely points out is that the ventilation and perfusion of the lung is not homogenous. Just as importantly, an inhaled breath is not homogenously distributed. Assuming that the patient inhaled to TLC in both instances, this may mean that the lower volume of the first session was preferentially distributed to the more highly perfused portions of the lung while during the second session the inhaled volume was distributed to both high and low perfused areas of the lung.
This doesn’t rule out clinical changes but there were substantial performance issues between both sessions and the difference in DLCO is more likely attributable to this. It also means that a better quality test does not mean a higher DLCO.
These comparisons are limited by the fact that the tests were performed at least a couple months apart. There is also no easy way to track which test system each set of tests were performed on (it can be done but it requires a complicated SQL query that must be run for each individual test) and my lab has six test systems that can perform DLCOs. In a sense though, that’s the point. Unless a PFT Lab has only one DLCO test system then a patient’s testing will usually be performed on whatever system is available and convenient. It’s also the point since the daily calibrations (and other quality control) are supposed to make sure that testing is accurate and repeatable regardless of which test system is being used.
Interestingly, while searching for changes in DLCO over the last couple of weeks what I found in most instances was that these changes were accompanied by changes in spirometry and/or lung volumes, and the direction of the changes were similar. When there were changes in DLCO without changes in spirometry, the majority were similar to the first example in that the primary change seemed to be in CO uptake alone and not in test performance. The next most common problem were changes in test performance and as can be seen from above sometimes even a relatively small change in performance can lead to a significant change in DLCO. There were actually remarkably few tests that were suspicious for gas analyzer problems and this reassures me that our equipment is in better shape than I expected.
DLCO results often rise and fall for reasons that are not completely clear. Many of the possible physiological causes for this such as cardiac output, capillary blood volume, the distribution of the inhaled volume and ventilation-perfusion mismatching cannot be measured directly. I was cautiously pleased to see that more often than not DLCO results did not change when there was no significant change in spirometry and/or lung volumes and this is despite the fact that the tests were likely performed on different systems. I think that one key to this is that DLCO results are usually averaged but the other is the constant calibration that the testing systems undergo and the highly standardized way in which the DLCO is performed.
References:
Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standarisation of lung function testing. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J 2005; 26: 720-735.
Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standarisation of lung function testing. Interpretive strategies for lung function tests. Eur Respir J 2005; 26: 948-968.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License

Richard , when i test Dlco in interstitial lung disease patients, i always get close reading within 5% some times dead-on as the first trial. but among asthmatics and normal’s always there is a discrepancy may be because of muller or valsalva maneuver which happens unknowingly .
Gilbert –
Why do you think your asthmatic and normal patients are performing Muller or Valsalva maneuver and not your interstitial lung disease patients? Offhand I’d say that Muller maneuvers (negative airway pressure) are less likely to occur than Valsalva maneuvers (positive airway pressure) but since most of the time people perform both of these maneuvers with a closed glottis it’s hard to tell that they’re happening with any certainty. I’m not saying they’re not happening and actually suspect that patients frequently perform the DLCO test with a mild Valsalva maneuver, just asking what leads you to suspect it and why the difference between patients.
– Richard
Richard..may be because their stiff lungs , the diffusing gas may be evenly distributed inside the lungs?? that may be the reason we get a better results on interstitial lung disease. thats my best guess