Recently I was reviewing a report that included helium dilution lung volumes. What caught my eye was that the TLC and the FRC didn’t particularly fit in with the results from the other tests the patient had performed.
| Test: | Observed: | %Predicted: |
| FVC: | 2.83 | 114% |
| TLC: | 3.03 | 71% |
| FRC: | 0.88 | 39% |
| RV: | 0.09 | 5% |
| SVC: | 2.93 | 118% |
| VA: | 3.64 | 88% |
When compared to the FVC and the VA (from the DLCO test) the lung volumes are significantly lower. In particular the FRC and RV are markedly reduced. This is somewhat unusual for helium dilution lung volume since most errors usually cause FRC, RV and TLC to be over-estimated instead of being under-estimated. When I checked the other reports for the day I found that two other patients that had had their lung volumes measured on the same test system also had a TLC, FRC and RV that were noticeably reduced. Obviously we had some kind of equipment problem with that test system but it took a bit of sleuthing before I found out what had happened.
Like all lung volume tests, the helium dilution technique produces a lot of numbers, most of which are not included on the report. One of the first things I did was to call up the within-test data (our test systems store data every 15 seconds during the test and re-calculate FRC each time).
| Time: | FRC, Liters | He conc. (%) | Ve (L./min.) | Vt, Liters |
| 0:15 | -1.00 | 9.71 | 6.16 | 0.21 |
| 0:30 | 0.06 | 8.87 | 10.1 | 0.59 |
| 0:45 | 0.43 | 8.61 | 11.76 | 0.78 |
| 1:00 | 0.69 | 8.44 | 9.05 | 0.72 |
| 1:15 | 0.76 | 8.39 | 8.18 | 0.74 |
| 1:30 | 0.79 | 8.37 | 8.32 | 0.59 |
| 1:45 | 0.82 | 8.36 | 8.15 | 0.62 |
| 2:00 | 0.83 | 8.35 | 7.79 | 0.65 |
| 2:15 | 0.86 | 8.33 | 5.51 | 0.62 |
| 2:30 | 0.87 | 8.32 | 5.34 | 0.63 |
| 2:45 | 0.88 | 8.32 | 0 | 0 |
When looking at this it was immediately evident there was a problem because the initial FRC was negative and this shouldn’t be possible. About the only way that helium dilution lung volumes can normally be underestimated is if the test is terminated way too early and the negative FRC ruled this out. It also narrows down the possible problems, but I had to think for a while and in doing so had to go back to the basics of the helium dilution test.
Helium dilution used to be the most common method for measuring lung volumes, but it requires a closed-circuit test system with a volume displacement spirometer. Most current test systems are open-circuit flow sensor-based systems and lung volumes are usually measured by nitrogen washout (or by plethysmography). Nevertheless, there are a couple of closed-circuit systems still being manufactured and there are a fair number of these systems still in service.
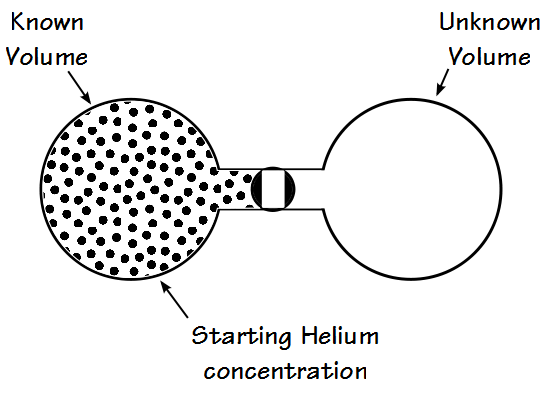
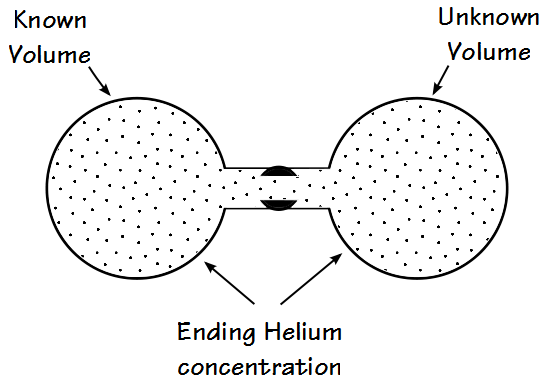
The basic concept behind the helium-dilution method is very simple and depends on the fact that helium is an inert and (and more importantly) insoluble gas. The dilution test could work with any highly insoluble gas but helium is relatively cheap and it’s easy to measure with a high degree of linearity (and reasonable accuracy) using an inexpensive katharometer (thermal conductivity) gas analyzer. You start with a system that has a known volume and a known concentration of helium:
You then connect the known system to another one that has an unknown volume and where the concentration of helium is zero. When the helium concentration has equilibrated between both systems, there will be a new and lower concentration of helium.
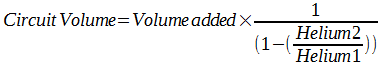
The unknown volume can then be calculated by:
Where:
Volume1 = original system volume
Volume2 = unknown volume
Helium1 = original helium fractional concentration
Helium2 = ending helium fractional concentration
When measuring lung volumes it’s a little more complicated than this, and there are a lot more steps in the process. One reason for the number of steps is that although katharometers tend to be highly linear unless they are calibrated with a known concentration of helium they aren’t necessarily all that accurate. Fortunately, linearity is far more important than accuracy and that is because the ratios of different helium concentrations can be used for the various calculations.
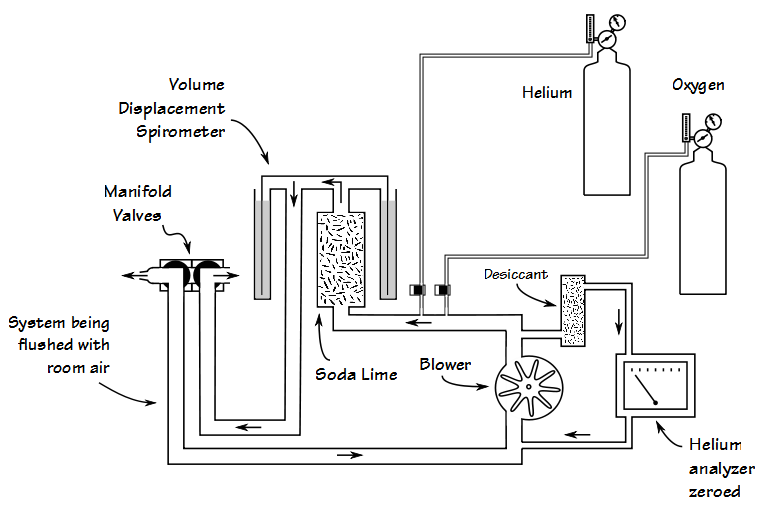
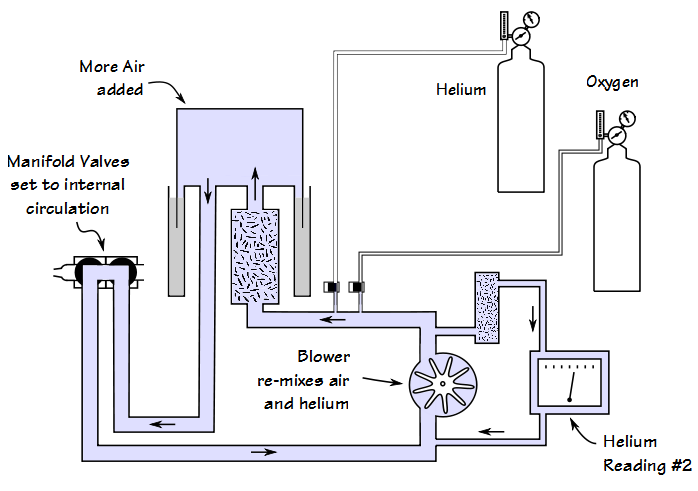
Stage 0: The closed-circuit is first flushed with air and the helium analyzer is zeroed.
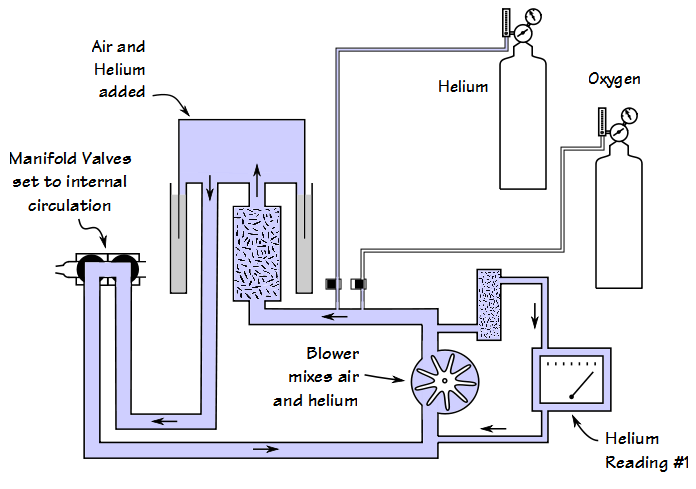
Stage 1: The manifold valves close the circuit off from external circulation. Air and helium are then added to the closed circuit and after the helium concentration has equilibrated throughout the circuit, the first helium reading is taken.
Stage 2: A specific volume of air is added to the closed circuit and a second helium reading is taken after the helium concentration has re-equilibrated.
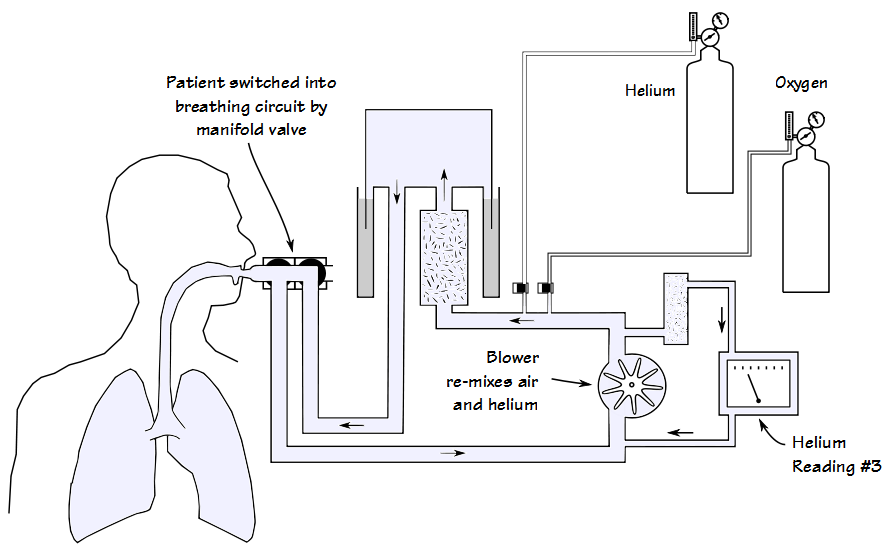
Stage 3: The patient goes on a mouthpiece and is switched into the closed circuit at end-exhalation. After several minutes of quiet breathing the helium concentration reaches a new equilibration and the third helium reading is taken.
FRC is then calculated from:
The volume of the closed-circuit at the end of stage 2 can also be calculated from ratios. Specifically:
So when you are done with a test you have a number of helium readings and a circuit volume. When I looked at these, and compared them to those from a patient whose helium dilution lung volumes looked okay and had been tested on a different system, there really wasn’t much difference:
| Low LV: | Normal LV: | |
| Helium1: | 12.31% | 12.46% |
| Helium2: | 9.87% | 9.99% |
| Helium3: | 8.32% | 8.23% |
| System Volume (L): | 10.24 | 10.22 |
One of the possibilities I considered was that helium was slowly leaking into the closed-circuit during the test. A leak would decrease the change in helium concentrations during equilibration and therefore decrease the calculated FRC, but the helium3 readings didn’t appear to be all that different between patients and test systems.
In order to be sure however, I asked one of the techs to do their own lung volumes on the test system in question but specifically asked them wait a couple of minutes between the time the system had finished setting itself up and the time they started the test. If there was a slow leak then waiting would cause the initial helium reading during the test to be higher than the helium2 reading. That turned out not to be the case and the tech’s FRC and TLC were pretty much the same as the last time they did their biological QC.
When calculating FRC you also need to subtract the system dead space (valve manifold + mouthpiece filter) so it was possible that somebody had inadvertently changed this (not supposed to be possible since you need administrative rights to do this, but still worth checking). If the dead space had somehow been set to somewhere between 0.5 and 1.0 liters that would explain both the initially negative and the reduced FRCs. When checked, these values had not been changed, however.
That didn’t mean there hadn’t been a glitch of some kind so I went into the database and looked at all the helium dilution FRC test records from that day. When I did this I found out two things. First, the mouthpiece filter dead space was in the FRC database records and it hadn’t been changed. Second however, the valve manifold dead space was not in the database records and this raises an interesting question of where it is being stored and retrieved from. There are several possibilities; that it is stored and retrieved from individual test systems, which means that if the results were retrieved on a different test system that had a different valve manifold dead space, would the calculated FRC be different? Or was the valve manifold dead space being retrieved from a different test (DLCO?). Or is it possible that the programmers didn’t think valve manifold dead space was an issue in the helium dilution FRC calculations? This isn’t in the manual (of course it isn’t, why would you expect testing details like this to be there?) so it’s a question I’ll have to follow up on sometime in the future.
When looking at the FRC database records however, one value immediately stood out, and that was the switching error. There was a marked increase in the switching error for all the patient’s whose FRC and RV were low.
| Low LV: | Normal LV: | |
| Switching Error (L): | 1.15 | 0.05 |
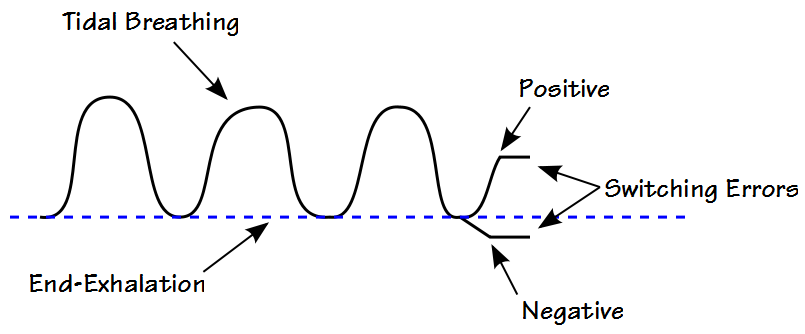
Switching error is the difference between the patient’s tidal end-exhalation volume and the volume where they were switched into the closed-circuit. It’s a positive number if the patient is switched in above the end-exhalation baseline, and negative if below.
Subjects are supposed to be switched into the closed-circuit as close to FRC as possible so the switching error should be close to zero, but in this case it was a lot closer to a liter. It’s unlikely that this is actually what happened for a couple reasons. First, the patient’s tidal breathing was closer to 0.50 L so even if they were switched into the circuit at end-inhalation the switching error still wouldn’t have been as high as it was. Second, the technician performing the tests has more than 10 years of experience and this is not the kind of error they would make, particularly not on three patients in a row.
Unfortunately, even though the system reports the switching error, it does not store any of the baseline tidal breathing so it’s not possible to go back and check to see if the switch-in was performed correctly or not. Since this problem has not showed up again since that day I am far more inclined to believe it was a transient glitch of some kind, either in the test system software or its hardware.
When I corrected the patient’s FRC, RV and TLC for the switch-in error the results were far more believable. This was an interesting problem that I had not noticed previously. That doesn’t mean it hasn’t happened before, just that I haven’t noticed it. In the future however, every time I look at the raw data for helium dilution lung volumes I will check to make sure the initial FRC value is not negative and that the switching error is within reasonable limits.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License

Richard
Interesting. I know some systems ‘correct’ for switch-in error up to a certain vol, and notify the tech in some fashion.
Mike
Mike –
Our systems do correct the FRC by subtracting the switch-in error (which is sort of the problem) but they don’t notify the tech if it’s too high.
– Richard
I didn’t understand this comment:
“About the only way that helium dilution lung volumes can normally be underestimated is if the test is terminated way too early”
I usually teach that obstructive lung disease is a fairly common cause of underestimating He-dilution lung volumes due to incomplete mixing.
Daniel –
It is commonly thought that gas dilution lung volume measurements will underestimate TLC when there is airway obstruction but this isn’t really supported in the literature. In particular, please refer to O’Donnell CR, Bankier AA, Stiebellehner L, Reilly JJ, Brown R, Loring SH. Comparison of plethysmographic and helium dilution lung volumes: which is best for COPD? Chest 2010; 137: 1108-1115. This showed that helium dilution lung volumes matched CAT scan volumetry better than plethysmography and that in fact TLC was systematically overestimated by plethysmography.
Although plethysmography is often considered the “gold standard” of lung volume measurement it routinely overestimates TLC in the presence of airway obstruction (which is because plethysmography assumes that mouth pressure = alveolar pressure and this tends not to be true when there is airway obstruction). Many clinicians and researchers have considered this overestimation to be a sign of gas trapping which is probably why gas dilution techniques got the reputation for underestimating TLC but this isn’t necessarily true at all.
Regards, Richard