I was reviewing a spirometry report last week and when I went to compare the results with the patient’s last visit I noticed that the FVC and FEV1 hadn’t changed significantly. However, the previous results were from 2009 and when the percent predicted is considered there may have been a significant improvement.
| 2009 | Observed: | %Predicted: |
| FVC: | 2.58 | 87% |
| FEV1: | 1.60 | 72% |
| FEV1/FVC: | 62 | 82% |
| 2016 | Observed: | %Predicted: |
| FVC: | 2.82 | 104% |
| FEV1: | 1.65 | 82% |
| FEV1/FVC: | 59 | 79% |
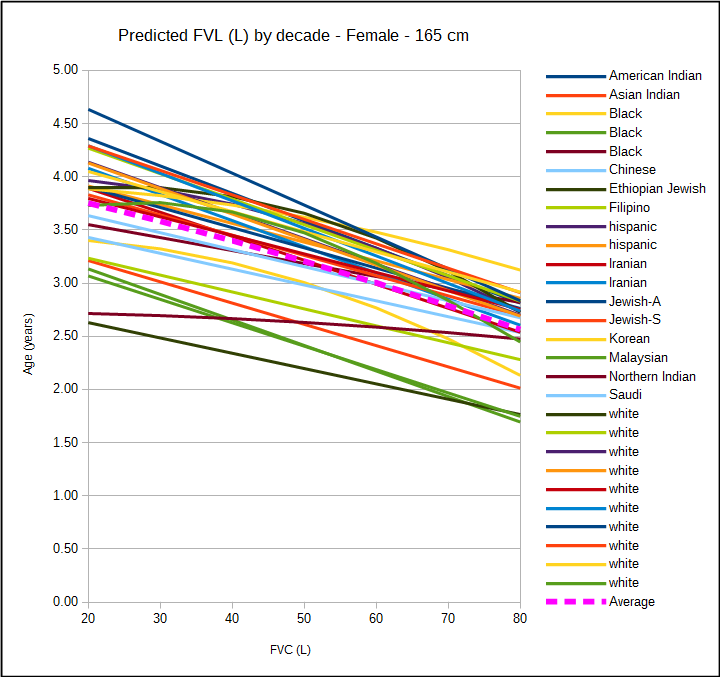
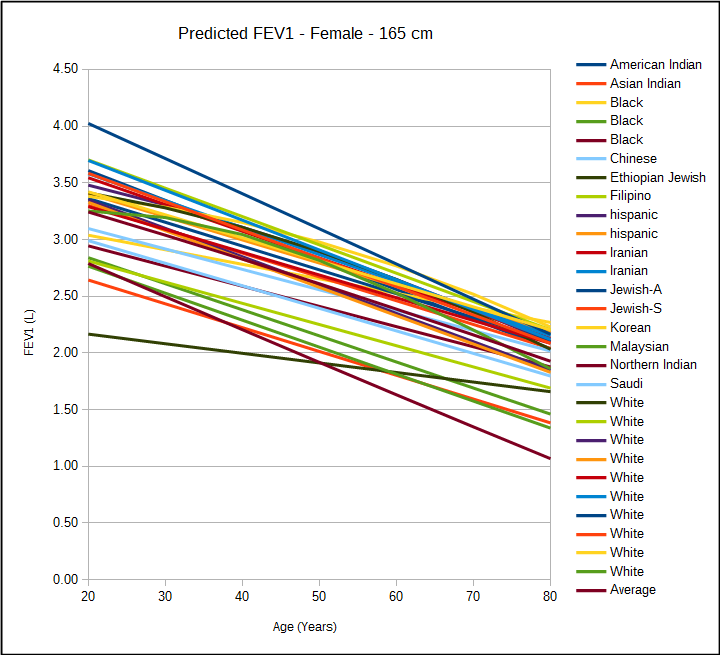
The answer to whether or not there was an improvement would appear to depend on what changes you’d normally expect to see in the FVC and FEV1 over a time span of 7 years. The FVC and FEV1 normally peaks around age 20 to 25 and then declines thereafter.
[more]
The rate at which FVC and FEV1 declines shown by reference equations comes from cross-sectional studies.
Longitudinal studies have often indicated that the rates of decline are different, and often lower than, those from cross-sectional studies. The reasons for these differences has been variously attributed to the learning effect, cohort effects (i.e. dependence on the year of birth rather than aging per se), and differences in study populations. In addition more than one longitudinal study has noted that returning participants are usually better educated with better health. Perhaps just as importantly returning participants are alive and sufficiently capable, mentally and physically, of performing acceptable quality spirometry.
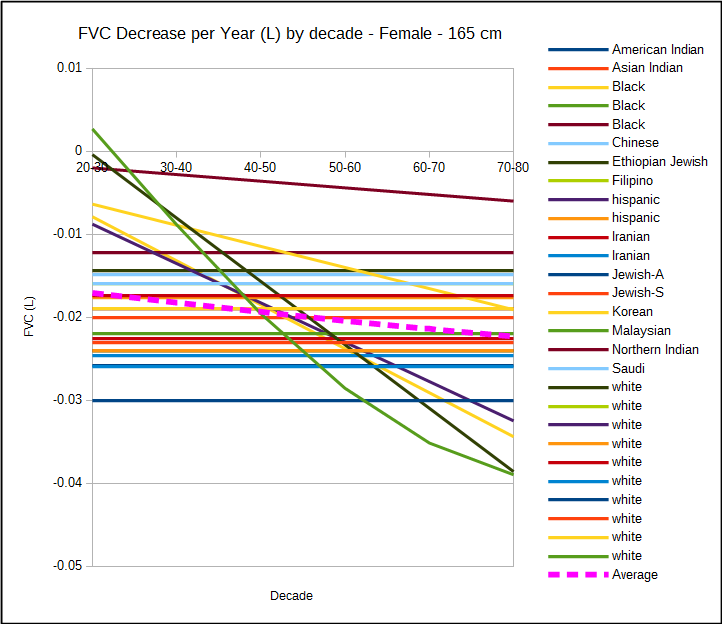
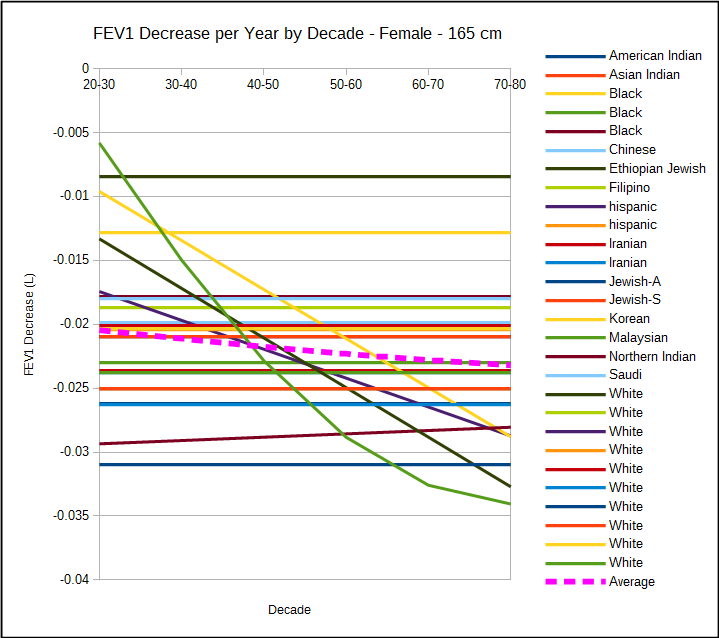
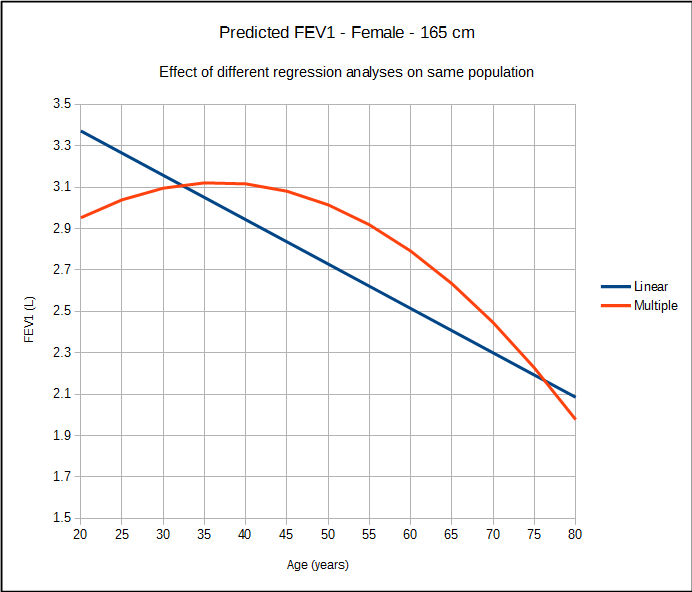
One relatively early finding from longitudinal studies was that the rate of decline accelerates as age increases and this is not evident in most cross-sectional studies. This is at least partially due to the type of statistical analysis that is performed. Linear regression is the most commonly used analytic tool but when the same population is studied with multiple step-wise regression analysis this pattern becomes more evident.
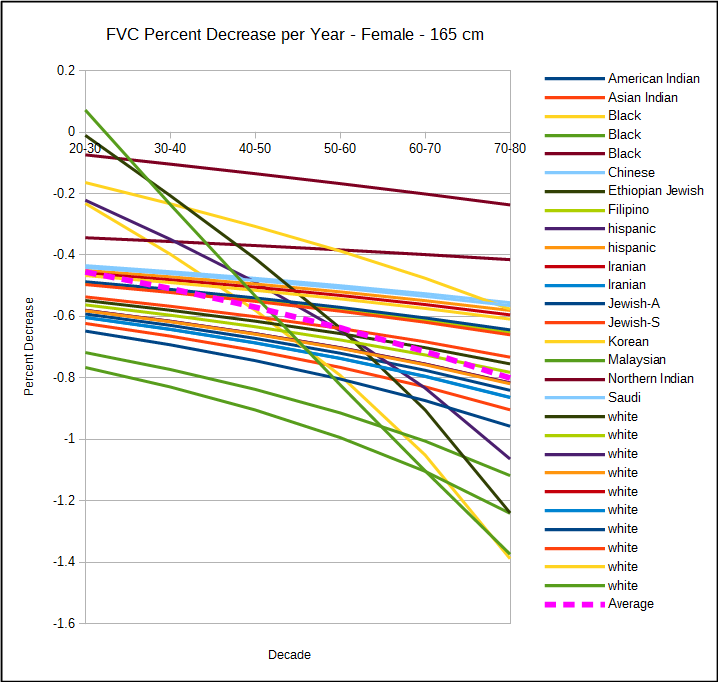
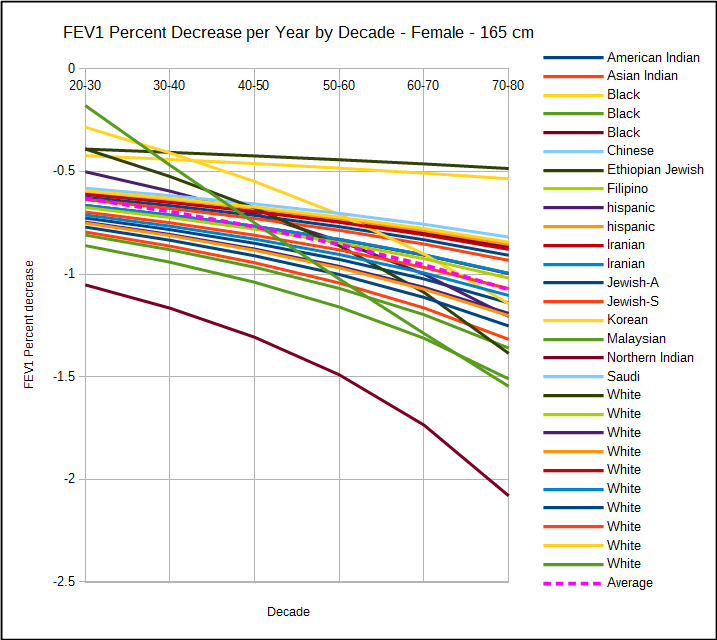
This also means that the rate of decline in FVC and FEV1 from any given longitudinal study are dependent on the demographics of the study population and what type of analysis is performed. For this reason, the reported rates of decline in FEV1 in non-smokers ranges from -10 ml/year to -56 ml/year. This also means that the rates of decline between cross-sectional and longitudinal studies although differing when compared individually are overall fairly similar.
One important point, and this applies to both cross-sectional and longitudinal studies, is that as FEV1 declines normally, the annual decrease when measured as a percent change increases.
Multiple longitudinal studies have shown (not surprisingly) that the rate of decline in both FVC and FEV1 is higher (usually at least double the rate) for smokers than non-smokers or ex-smokers. They have also shown that the rate of decline is also higher for individuals with emphysema, COPD, asthma, cardiovascular disease, cardiac disease or with an increasing BMI. At least one study showed that the rate of decline was greater for Caucasians than for blacks and another showed that rate of decline was greater for taller individuals than for shorter (which is perhaps why a number of studies report the rate of decline as ml/m3). Interestingly, although the use of bronchodilators (either short-acting or long-acting) does not appear to affect the rate of decline at least one study showed that the use of statins decreased the rate of decline among non-smokers, smokers and quitters.
Since there the rate of decline in FVC and FEV1 would appear to be an important factor in a given individual’s clinical management, why isn’t it routinely measured? The primary reason is that more than one study has shown that the normal level of year-to-year variability in FEV1, even in healthy subjects, is many times higher than the rate of decline. For this reason testing must be performed regularly over long periods of time before a rate of decline can be determined with any reliability. In addition, patients that return to the PFT lab are often seen intermittently and often only during periods of ill health. This adds a level of variability to spirometry results that make it far more difficult to determine a meaningful rate of decline.
Getting back to the original question, is the lack of change actually an improvement? In one sense, the patient has probably had some clinical improvement, but when considering the amount of routine visit-to-visit variability in test results, probably not enough to be remarked about, at least not over a 7 year period. If it was considered over a longer time period however, there has to be a point at which no change is both statistically and clinically significant. At the present time both the ATS/ERS and the ACOEM state that when considering changes in FEV1 over the course of 1 year, that a 15% decrease is clinically important. As a starting point therefore, 15% seems far enough above the “noise” level that when comparing results separated by enough time that the FVC or FEV1 should have decreased by 15% but instead remained the same, then there has probably been significant improvement.
References:
Alexeeff SE, Litonjua AA, Sparrow D, Vokonas PS, Schwartz. Statin use reduced decline in lung function. VA Normative Aging Study. Amer J Respir Crit Care Med 2007; 176: 742-747.
Anthonisen NR, Connett JE, Murray RP. Smoking and lung function of Lung Health Study participants after 11 years. Amer J Respir Crit Care Med 2002; 166(5): 675-679.
Burrows B, Lebowitz MD, Camilli AE, Knudsen RJ. Longitudinal changes in forced expiratory volume in one second in adults. Methodological considerations and findings. Amer Rev Respir Dis 1986; 133: 974-980.
Carey IM, Cook DG, Strachan DP. The effects of adiposity and weight change on forced expiratory volume decline in a longitudinal study of adults. Int J Obesity 1999; 23: 979-985.
Cibella F, Cuttitta G, Bellia V, Bucchieri S, D’Anna S, Guerrera D, Bonsignore G. Lung function decline in bronchial asthma. Chest 2002; 122(6): 1944-1948.
Griffith KA, Sherrill DL, Siegel EM, Manolio TA, Bonekat HA, Enright PL. Predictors of loss of lung function in the elderly. The cardiovascular health study. Amer J Respir Crit Care Med 2001; 163(1): 61-68.
Hnizdo E, Yu L, Freyder L, Attfield M, Lefante J, Glindmeyer HW. The precision of longitudinal lung function measurements: monitoring and interpretation. Occup Environ Med 2005; 62: 695-701.
Hnizdo E, Sircar K, Yan T, Harber P, Fleming J, Glindermeyer HW. Limits of longitudinal decline for the interpretation of annual changes in FEV1 in individuals. Occup Environ Med 2007; 64: 701-707.
Kerstjens HAM, Rijcken B, Schouten JP, Postma DS. Decline of FEV1 by age and smoking status: facts, figures and fallacies. Thorax 1997; 52: 820-827.
Peat JK, Woolcock AJ, Cullen K. Decline of lung function and development of chronic airflow obstruction: a longitudinal study of non-smokers and smokers in Busselton, Western Australia. Thorax 1990; 45: 32-37
Ryan G, Knuiman MW, Divitini ML, James A, Musk AW, Bartholomew HC. Decline in lung function and mortality: The Busselton Health Study. J Epidemiol Community Health 1999; 53: 230-234

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License