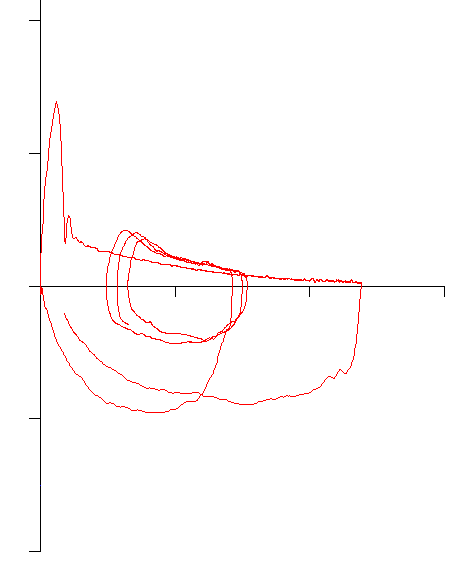
One of the more recognizable flow-volume loop contours is the one associated with severe airway obstruction. Specifically, this type of loop shows an abrupt decrease in flow rate following the peak flow with a more gradual decrease in flow rates during the remainder of the exhalation.
This abrupt decrease in flow rates was first described on a volume-time curve and the inflection point was called a “kink” but this point also corresponds with the inflection point on the flow-volume loop. This feature has also been called a “notch” or a “spike” but a number of researchers have called this the Airway Collapse pattern (AC) and it is more formally defined as a sharp decrease in flow rate from peak flow to a discontinuity point at less than 50% of the peak flow and occurring within the first 25% of the exhaled vital capacity.
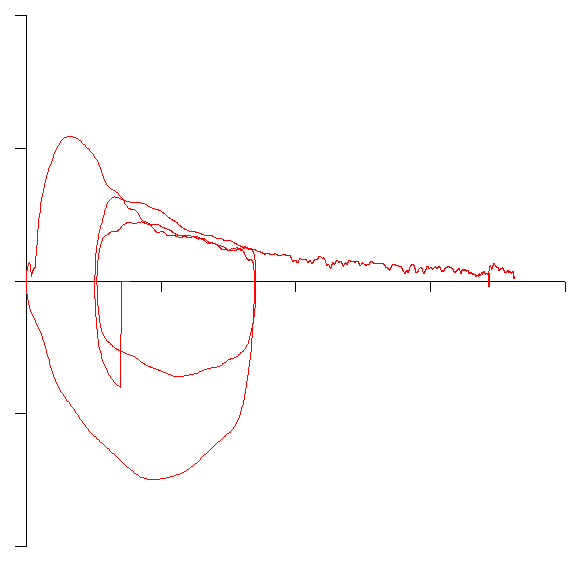
Although the AC pattern is associated with severe decreases in FEV1 and the FEV1/FVC ratio, its presence cannot be predicted by either the FEV1 or FEV1/FVC ratio. For example, compared to the above example the following loop actually has a slightly lower FEV1 and FEV1/FVC ratio:
The AC pattern is a consequence of a loss of elastic recoil in the lung and dynamic airway compression during a forced exhalation. More specifically numerous researchers have shown that the AC pattern is closely associated with emphysema. When groups of individuals with similar FEV1’s and FEV1/FVC ratios those with the AC pattern were more likely to have more gas trapping and hyperinflation, a higher airway resistance and to have a lower DLCO than those with a more curvilinear exhalation.
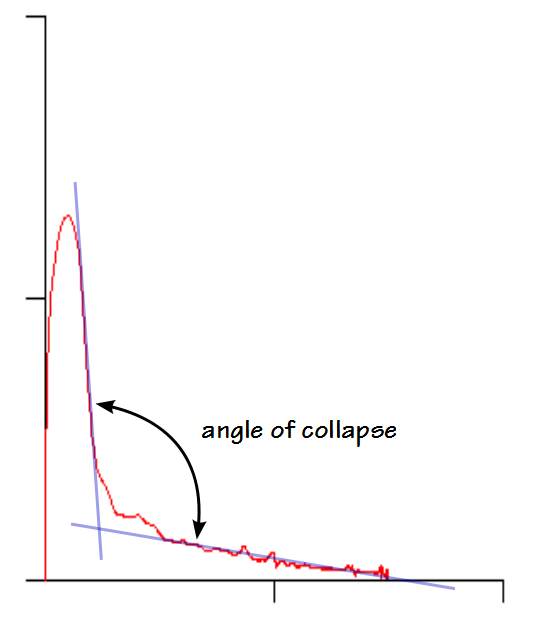
A recent study used a computer algorithm to place a pair of regression lines on flow-volume loops. Best fit was determined by mean square error and the angle between the two lines was measured. This angle was called the angle of collapse and using this approach, a lower angle implies a sharper “kink”.
When they compared FEV1, FEV1/FVC ratio, DLCO and the presence (defined as an area of hypovascular low attenuation) and amount of emphysema (defined as the percent of voxels with an X-ray attenuation value below -950 HU) from CT scans they found that angles of collapse below 131º had a positive predictive factor of 95.5% for the presence of emphysema. As importantly they also found that there was a direct correlation with the angle of collapse and the severity of emphysema. Individuals with lower angles of collapse uniformly had lower FEV1’s, lower FEV1/FVC ratios, lower DLCO’s and a greater amount of emphysema as assessed by their CT scan. They also found that lower angles of collapse had a higher predictive value for emphysema than did a low DLCO or a low FEV1/FVC ratio.
Although it has been hypothesized that decreased elasticity is a major factor in the presence of the AC pattern there has been somewhat equivocal evidence to support this. Of the two studies that looked at compliance, one showed no statistical difference in compliance in patients with and without the AC pattern. The second study showed significantly lower elasticity in patients with the AC pattern when compared to those with a curvilinear patter. There was however, a notable difference between the two studies. In particular the first study looked at individuals with similarly reduced FEV1’s and FEV1/FVC ratios whereas the second study only considered the presence or absence of the AC pattern and in addition the authors of the second study criticized (mildly) the statistical methods of the first study. This is not to say that individuals with the AC pattern don’t have decreased elasticity just that it may not be the sole factor for the development of the AC pattern.
Patients that have an AC pattern on their flow-volume loop rarely, if ever, revert to a more curvilinear flow-volume loop contour. The persistence of the AC pattern implies that the physiological changes that cause it to occur are likely irreversible. Having said that, at least one study showed that an individual with a curvilinear flow-volume loop shifted to an AC pattern during a methacholine challenge and reverted to curvilinear afterwards.
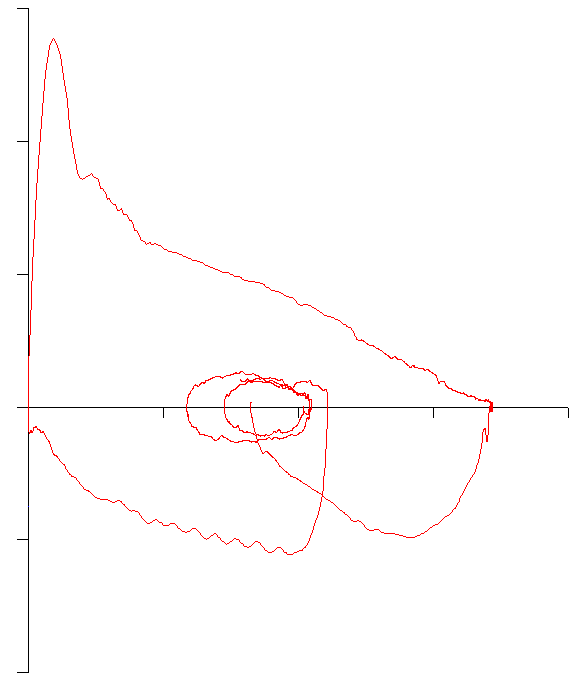
The formal definition of the AC pattern includes a decrease in flow to less than 50% of the PEF. Although this is reasonable as a working definition, it is somewhat arbitrary. There are a number of patients whose flow-volume loop shows a “kink” but at flow-rates above 50% of the PEF. For example, this patient had a mild OVD (the FEV1/FVC ratio was 81% of predicted and FEV1 83% of predicted):
So an interesting question, and one that does not seem to have been studied, is whether this small kink is an early sign of emphysema, a possible sign of a loss of elasticity or whether it just a normal variant in mild airway obstruction. I will mention that this patient had signs of gas trapping (elevated FRC, RV and RV/TLC ratio) despite having only mild airway obstruction but as a sample of one, it is hardly indicative of broader patterns.
A reduced FEV1 and FEV1/FVC ratio indicates the presence of airway obstruction, and the degree by which they are reduced correlates with the severity of the airway obstruction. The FEV1 and FEV1/FVC ratio alone however, cannot differentiate between asthma, chronic bronchitis and emphysema. The AC pattern is easily recognizable and appears to be highly specific to emphysema. Importantly, there is a good correlation between the “kinkiness” of a flow-volume loop and the severity of the emphysema. Although measuring the angle of collapse appears to be a way to quantify “kinkiness” (and would allow for an automated interpretation in office spirometers) I am concerned that it attempts to match straight lines to what are, in reality, curves. Having said that, compared to other approaches to the graphical analysis of flow-volume loops it appears to be a better way to describe the AC pattern (although I’m somewhat doubtful that it’s a relevant approach to analyzing curvilinear flow-volume loops without an inflection point).
Note: While researching flow-volume loops I’ve found that there is a marked lack of consensus in the words used to describe them. Our eyes may be good at recognizing contours but our ability to describe and communicate what we see is somewhat limited. Are these flow-volume loops kinky, do they have a notch, is it a sharp inflection point, is it a spike or are they AC patterns? Are more curvilinear flow-volume loops curved, scooped, coved or concave (or depending on how you look at it, convex)? Are loops from individuals without airway obstruction flat, convex or is normal sufficient, and is that a shoulder or a knee? Maybe it’s not important since we do understand these terms reasonably well but it does seem to me that this is one area we should be able to be more precise.
References:
Campbell AH, Faulks LW. Determinants of expiratory airflow obstruction in patients with chronic airways obstruction. Thorax 1973; 28(1): 48-54.
Healy F, Wilson AF, Fairshter RD. Physiologic correlates of airway collapse in chronic airflow obstruction. Chest 1984; 85(4): 476-481.
Jayamanne DS, Epstein H, Goldring RM. Flow-volume curve contour in COPD: correlation with pulmonary mechanics. Chest 1980; 77(6): 749-757.
Saltzman HP, Ciulla EM, Kuperman AS. The spirographic “kink”. A sign of emphysema. Chest 1976; 69(1): 51-55.
Topalovic M et al. Computer quantification of airway collapse on forced expiration to predict the presence of emphysema. Respiratory Research 2013; 14: 131

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License