I’ve been interested in ventilation inhomogeneity for a while and as ways to measure it I have looked at VA/TLC ratios, the Lung Clearance Index (LCI) and the phase III slope of the single-breath N2 washout (SIIIN2). All of these tests are able to provide some information about ventilation inhomogeneity but each has their own limitations and just as importantly although their results have a relatively clear relationship with ventilation inhomogeneity it’s not quite as clear what exactly it is they are measuring. A friend recently pointed me to an on-line article in Chest that discusses the dual-tracer single-breath washout test in patients with COPD. The apparent advantage of this test is that it is able to provide information about the site of the ventilation inhomogeneity. Although dual tracer gases have been used to study airway function for over 50 years the limitation of this technique has been the need to use a mass spectrometer. Some recent advances in technology have made it possible for this type of testing to be performed with a significantly less expensive gas analyzer and this has revived an interest in the dual-tracer gas single-breath washout (DTG-SBW).
The two tracer gases in question are Helium and Sulfur Hexaflouride (SF6). Helium has a density of 4 gm/mol and the density of SF6 is 146 gm/mol, and it is the difference in densities between these two inert and insoluble gases that make this test useful. In order to understand why we need to revisit to the anatomy of the terminal airways.

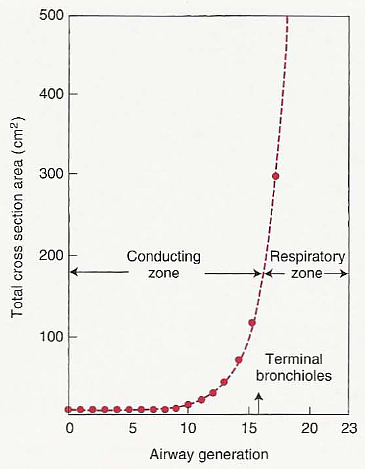
From Osborne S. Airway resistance and airflow through the tracheobronchial tree. www.SallyOsborne.com.
As the airways branch from the trachea towards the alveoli up to the fifth generation the cross-sectional area remains about the same (which is also why the majority of airway resistance occurs within the first five generations) but after this each succeeding generation shows an increase in cross-sectional area.
When air flows into the lung during an inhalation, air velocity is highest in the trachea but because of the increase in cross-sectional area of the airways air velocity decreases as it travels deeper into the lung. Somewhere around the respiratory bronchioles and acinus the convective air velocity is so low that gas molecules travel faster by diffusion than they do by convection. The point at which this occurs has been called the diffusion wavefront. Up to the diffusion wavefront convective transport will be equal regardless of gas density but the speed or rate of diffusion in any given gas is dependent on its density. Heavier molecules diffuse more slowly than lighter ones and the diffusion coefficient for helium is approximately 6 times higher than it is for SF6. This means that the diffusion wavefront for helium usually occurs in the terminal or respiratory bronchioles and for SF6 it usually occurs somewhere inside the acinus.
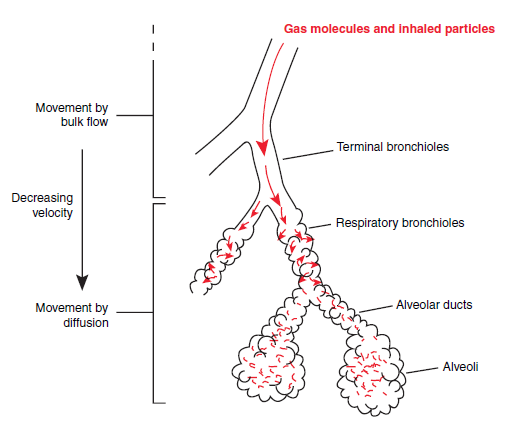
From Schwartzstein RJ, Parker MJ. Respiratory physiology. A clinical approach. Published by Lipincott, Williams and Wilkins, 2006.
At the end of a tidal breath that contains helium and SF6 the difference in diffusion wavefronts causes the SF6 concentration to elevated in the terminal and respiratory bronchioles and for helium to be more evenly distributed through the bronchioles and the acinus. During exhalation therefore, the ratio between SF6 and helium will be highest at the beginning of exhalation and decrease thereafter. An increase in ventilation inhomogeneity in the terminal bronchioles (as opposed to the acinus) will therefore act to further separate the SF6 and helium and steepen the expiratory slope.
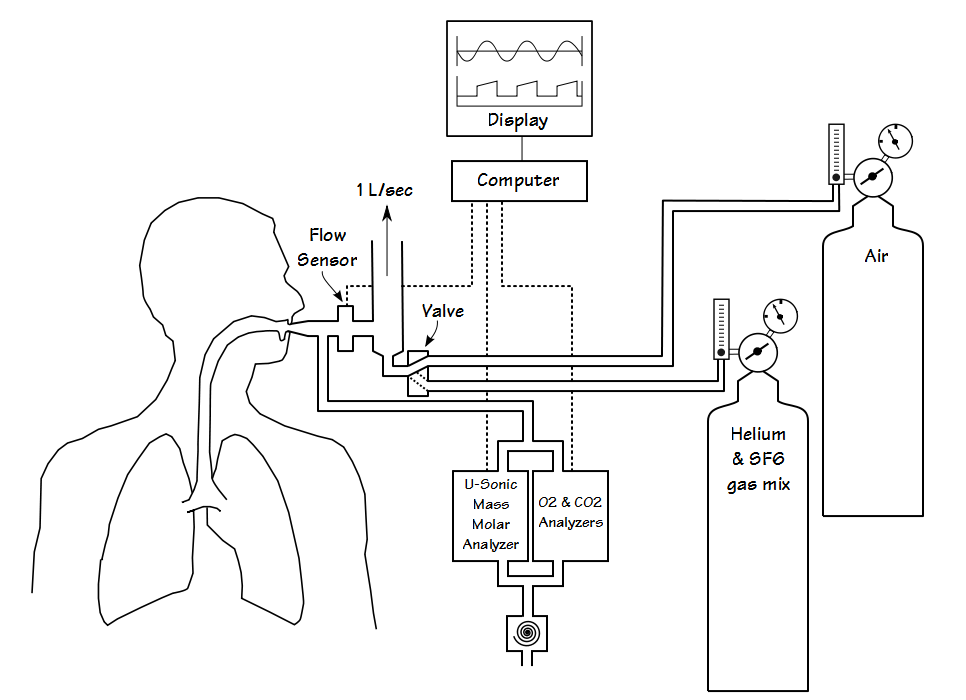
From Singer F, Stern G, Thamrin C, Fuchs O, Riedel T, Gustafsson P, Frey U, Latzin P. Tidal volume single breath washout of two tracer gases – A practical and promising lung function test. PLOS One 2011; 6(3): e17588, page 3]
The DTG-SBW is performed during tidal breathing and only over a single tidal breath. The subject breathes on a gas circuit with a flow sensor, O2 analyzer, CO2 analyzer and an ultrasonic mass molar analyzer. After several normal and reproducible tidal breaths the blow-by breathing circuit is switched from air to a mixture containing helium and SF6 and the subject takes a normal tidal breath. At end-inhalation the breathing circuit is switch back to air.
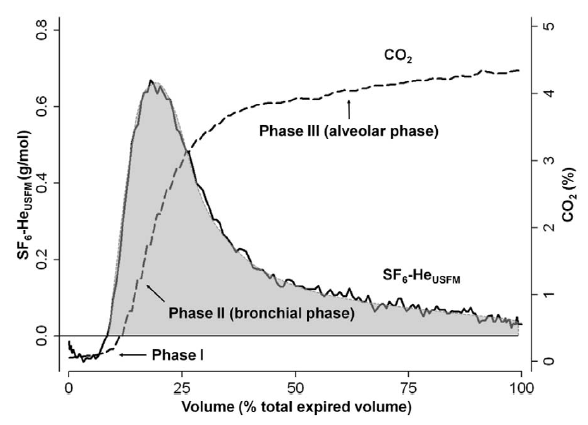
The ultrasonic mass molar analyzer measures gas density, not individual gas concentrations. For this reason the test gas mixture usually contains 5% SF6, 26.3% helium, 21% O2 and balance N2 which has a density that is essentially the same as air. During air breathing the changes in density that occur during exhalation are primarily due to CO2. After the inhalation of the DTG-SBW gas mixture the exhaled CO2 signal is used to subtract the contribution of CO2 to the exhaled gas density. This produces a calculated signal which primarily reflects the changes in the ratio between SF6 and helium.
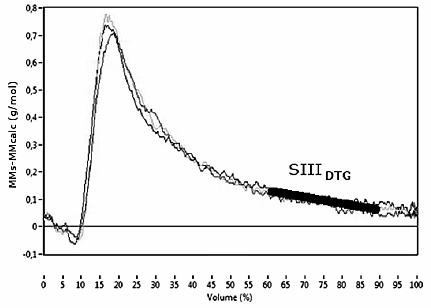
The measurement that is most commonly made from the more recent DTG-SBW tests is the slope of the SF6-Helium ratio between 60% and 90% or 65% to 95% of the exhaled tidal volume. This is usually termed the phase III slope and is most frequently designated the SIIIDTG. This value is usually normalized by multiplying it by tidal volume in order to make results from different breaths and different individuals comparable and this is designated as the SnIIIDTG. In the past however, the SIIIDTG has been taken from different volume spans such as 35% to 85% and although the overall conclusions are similar, the reported slopes may be different.
From Huseman K, Berg, Engel J, Pot J, Joppek C, Tao Z, Singer F, Schultz H, Kohlhaufl M. Double tracer single-breath washout: Reproducibility in healthy s
SIIIN2 and LCI appear to measure ventilation inhomogeneity at a global level whereas an elevated SIIIDTG is considered to show an increase in ventilation inhomogeneity at the acinar level. One point that is occasionally confusing is that strictly speaking the SIIIDTG is negative (i.e. sloping downwards) and so a lower slope usually means a steeper slope. This is in contrast to the positive phase III slope of the N2 washout where a lower slope usually refers to one that is flatter. Researchers however, often arbitrarily invert the SIIIDTG slope and report it as a positive value. This means its important to read carefully in order to be sure what changes are being discussed.
More than one study has showed that the SIIIDTG and SnIIIDTG results from children show a distinct difference between those with normal lungs and those with cystic fibrosis. One study, was able to show distinct improvements in SIIIDTG in cystic fibrosis patients following bronchodilator and chest physiotherapy and that these improvements were slightly more significant than the changes in FEV1. Another study indicated however, that SIIIDTG has a somewhat lower sensitivity and specificity than the LCI.
Studies in individuals with COPD also showed significant differences in SIIIDTG between between healthy subjects and those with COPD. Interestingly, one study that compared SIIIDTG with SIIIN2 showed that increased slopes from both correlated with decreases in DLCO, but that the SIIIN2 correlated with FEV1 whereas the SIIIDTG did not. In addition the SIIIN2 correlated with an elevated RV/TLC ratio (gas trapping) whereas the SIIIDTG correlated instead with an elevated TLC (hyperinflation).
Studies in individuals with asthma have also shown a correlation between FEV1 and the SIIIDTG. As importantly, they have shown that the terminal airways are a factor during bronchoconstriction in individuals with more severe asthma (or at least more hyperreactive airways).
One study in lung transplant patients where helium and SF6 washout curves and not the SF6-Helium ratio were analyzed showed that the helium phase III slope became steeper well in advance of the onset of bronchiolitis obliterans and better served as an early warning of this disorder than did spirometry.
The use of tidal breath washout in the SIIIDTG as opposed to the vital capacity washout used in the SIIIN2 are largely due to the observation that the phase III slope in a vital capacity maneuver is affected by large-scale and small-scale inhomogeneities that are at least partly dependent on gravity and airway closure. Research has shown that inhalations from FRC are less affected by gravity and other confounding effects, and maximizes the differences between convective and diffusive gas transport. One point that does not appear to have been addressed however, is that the ventilation that occurs during tidal breathing is not homogeneously distributed throughout the lung, even in healthy subjects. Admittedly, the SIIIN2 and the SIIIDTG both appear to partition individuals with airway disorders from healthy subjects equally well, and admittedly the type of ventilation inhomogeneity each measures is expected to be different, but unclear to me how well the SIIIDTG from a tidal breath extrapolates to the lung as a whole.
Although several studies have shown reasonably good inter-test and intra-test reproducibility at least one study showed that SIIIDTG was affected by expiratory flow rates and tidal volume. In particular the SIIIDTG became less steep when tidal volume and expiratory flow rates increased and this occurs even when the SIIIDTG is normalized for tidal volume. This effect has not been completely explained and may place a limit on the clinical significance of the SIIIDTG and the ability to assess changes over time and between individuals.
The ultrasonic mass molar gas analyzer is significantly less expensive than a mass spectrometer but its use still requires technical proficiency. Like the gas analyzers in a CPET system the mass molar gas analyzer, O2 and CO2 analyzers are time delayed relative to the flow signal at the patient’s mouth both due to gas transport and analyzer rise times careful attention must be made to synchronizing signals. One important point is that this type of analyzer does not measure the concentrations of individual gases, only the mass of the entire gas mixture. For this reason it can only measure the ratio of helium to SF6 and then only when careful attention is paid to subtracting the contribution CO2 makes to the mass of exhaled air. This also means that if the phase III slope of both helium and SF6 change by the same amount, then the slope of the SF6-Helium ratio will not change.
The DTG-SBW is an intriguing test that has the potential to provide more information about ventilation inhomgeneity than the LCI and SIIIN2. On the positive side it is easy to perform and only takes a short time to perform the test multiple times, both factors that makes it a test well suited to children. Despite the fact that the SIIIDTG appears to easily differentiate between healthy subjects and those with various airway disorders however, its clinical use is limited by the fact that there are at present no agreed-upon normal values. As importantly, it’s unclear what constitutes a clinically significant change and it’s unclear what changes in the SIIIDTG means in a clinical sense for the various airway disorders. I will also admit to having some reservations about the ultrasonic mass molar analyzer, partly for it’s need for a relatively high level of technical proficiency but also for its limitation in measuring only the SF6-He ratio. For these reasons the DTG-SBW is probably useful in a research setting, but its clinical utility, at least at this time, is probably quite limited.
Decades ago the study of obstructive lung diseases crystalized around the FEV1/FVC ratio and issues that had previously been murky were suddenly seen with a new clarity. Tests of ventilation inhomogeneity have the potential to provide an even more nuanced understanding of airway disorders but at the moment most of these tests measure effects that are at least one step removed from the actual physiological process with results expressed in ways that relate to the test (lung turnovers, phase III slopes) and not the underlying physiology. The use of two tracer gases with markedly different densities appears able to bring some needed clarity to ventilation inhomogeneity measurements but in order for the DTG-SBW to become a routine and useful measurement there needs to more work performed on correlating results with specific airway disorders and with specific changes in airway disorders. Just as importantly, a way will have to be found to express results in a way that makes the underlying physiology clear.
References:
Abbas C, Singer F, Yammine S, Casaulta C, Latzin P. Treatment response of airway clearance assessed by single-breath washout in children with cystic fibrosis. J Cystic Fibrosis 2013; 12: 567-574.
Boeck L, Gensmer A, Nyilas S, Stieltjes B, Re TJ, Tamm M, Latzin P, Stolz D. Single-breath washout tests to assess small airway disease in COPD. CHEST 2016, doi: 10.1016/j.chest.2016.05.019.
Estenne M, Van Muylem A, Knoop C, Antoine M. Detection of obliterative bronchiolitis after lung transplantation by indexes of ventilation distribution. Am J Respir Crit Care Med 2000; 162: 1047-1051.
Gustafsson PM, Ljungberg HK, Kjellman B. Peripheral airway involvement in asthma assessed by single-breath SF6 and He washout. Eur Respir J 2003; 21: 1033-1039.
Huseman K, Berg, Engel J, Pot J, Joppek C, Tao Z, Singer F, Schultz H, Kohlhaufl M. Double tracer single-breath washout: Reproducibility in healthy subjects and COPD. Eur Respir J 204; 44: 1210-1222.
Olfert IM, Prisk GK. Effect of 60º head-down tild on peripheral gas mixing in the human lung. J Appl Physiol 2004; 97: 827-834.
Osborne S. Airway resistance and airflow through the tracheobronchial tree. www.SallyOsborne.com.
Paiva M, Engel LA. Theoretical studies of gas mixing and ventilation distribution in the lung. Physiological Reviews 1987; 67(3): 750-796.
Robinson PD, et al. ERS/ATS Consensus Statement for inert gas washout using multiple- and single-breath tests. Eur Respir J 2013; 41: 507-522.
Schwartzstein RJ, Parker MJ. Respiratory physiology. A clinical approach. Published by Lipincott, Williams and Wilkins, 2006.
Singer F, Stern G, Thamrin C, Fuchs O, Riedel T, Gustafsson P, Frey U, Latzin P. Tidal volume single breath washout of two tracer gases – A practical and promising lung function test. PLOS One 2011; 6(3): e17588.
Singer F, Stern G, Thamrin C, Abbas C, Casualta C, Frey U, Latzin P. A new double-tracer gas single-breath washout to assess early cystic fibrosis lung disease. Eur Respir J 2013; 41: 339-345.
Van Muylem A, De Vuyst P, Yernault JC, Paiva M. Inert gas single-breath washout and structural alteration of respiratory bronchioles. Am Rev Respir Dis 1992; 146: 1167-1172.
Van Muylem A, Paiva M, Estenne M. Involvement of peripheral airways during methacholine-induced bronchoconstriction after lung transplantation. Am J Respir Crit Care Med 2001; 164: 1200-1203.
Weibel ER. “Geometry and dimensions of airways of conductive and transitory zones.” In Morphometry of the human lung. Published by Springer, 1963: 110-135.
West J. Respiratory physiology – The Essentials 7th edition, published by Lipincott, 2004.
Wilschut FA, Van der Grinten CPM, Lamers RJS, Wouters EFM, Luijendijk SCM. Intrapulmonary gas mixing and the sloping alveolar plateau in COPD patients with macroscopic emphysema. Eur Respir J 1999; 14: 166-171.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License