The single-breath DLCO maneuver can rightly be criticized as being an artificial maneuver that bears little resemblance to normal breathing. It is only by standardizing the maneuver that clinically relevant and reproducible results can be obtained. One important aspect of this standardization is the breath-holding period.
The single-breath DLCO maneuver begins with a subject exhaling to RV, followed by an inhalation of the test gas mixture to TLC and then a 10-second breath-holding period, ending with an exhalation during which a sample of alveolar air is collected. The initial choice of a 10-second breath-hold period was largely arbitrary and was selected in order to strike a balance between being a short enough period that for most patients to hold their breath, long enough to minimize the inspiratory and expiratory phases and long enough to allow for a sufficiently measurable amount of carbon monoxide to be taken up.
During the inspiratory phase of the DLCO maneuver, carbon monoxide uptake does not begin until the inhaled gas has passed both the test system’s and the subject’s anatomic dead space and reached the first functional alveolar-capillary unit. The full rate of carbon monoxide uptake will not occur until the diffusing gas mixture has reached all available alveolar-capillary units and these units have reached their maximum surface area. The rate of carbon monoxide uptake therefore increases throughout inhalation and reaches a maximum near TLC.
During the exhalation phase, carbon monoxide uptake continues even as the alveolar sample is being taken. For this reason the concentration of carbon monoxide at the beginning of the sampling period tends to be higher than at the end of the sampling period. The size of the washout volume and the alveolar sample volume, which to some extent determines how long a patient has to exhale before the acquisition of an alveolar sample is complete, will also have an effect on exhaled gas concentrations.
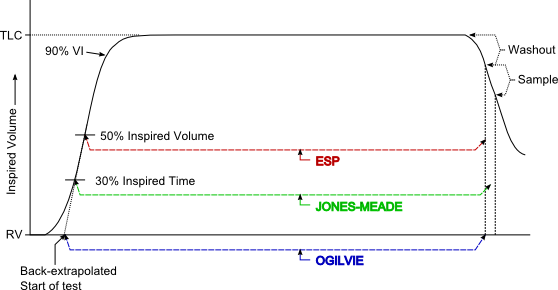
Because the point at which carbon monoxide uptake starts and the point at which it ends are to some degree indeterminate, several methods for standardizing the measurement of the single-breath DLCO breath-hold period have been developed. Of these, the Ogilvie method starts measuring the breath-hold period at the very beginning of inhalation and stops at the beginning of the alveolar sampling period. The Epidemiology Standardization Project (ESP) method, on the other hand, also stops at the beginning of the alveolar sampling period but instead starts measuring at 50 percent of the inhaled volume. Finally, the Jones-Meade method starts measuring at 30 percent of the inspiratory time and stops in the middle of the alveolar sampling period.
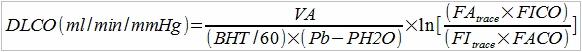
As a reminder, single-breath DLCO is calculated by:
A DLCO test measures the rate of CO uptake which is expressed as ml/min/mm Hg. For the same inspired and expired CO concentrations a shorter BHT would mean a quick uptake of CO has occurred and a longer BHT would mean a slow uptake of CO has occurred. When these different breath-hold measurement methods are applied to the same test results, the ESP method, which generates the shortest breath-hold time, has the largest calculated DLCO. The Ogilvie method, which generates the longest breath-hold time, has the smallest calculated DLCO. The Jones-Meade method tends to fall in between the ESP and Ogilvie methods in patients with normal lungs.
Both the Ogilvie and the ESP methods tend to overestimate DLCO when airway obstruction is present. This is because with airway obstruction it takes longer to get an alveolar sample. Both the Ogilvie and ESP methods stop measuring time at the beginning of the alveolar sampling period, even though some CO uptake may still be occurring. For this reason they tend to generate a shorter breath-hold time than may be appropriate. The Jones-Meade method however, includes some of the alveolar sampling time in the measurement of breath-hold time and therefore tends to have the least overestimation of DLCO in the presence of airway obstruction. It is for this reason that the ATS-ERS Statement on DLCO testing recommends the use of the Jones-Meade method.
Both the Ogilvie and Jones-Meade methods for measuring the beginning of the breath-hold period are time based, so it is important to know when inspiration begins and ends. Ideally the onset of inspiration should be rapid and easily recognizable. When it is less easy to determine the beginning of inspiration, the ATS recommends use of the standard back extrapolation technique to determine the onset of inspiration. The end of inspiration should also be clear and easily recognizable. When it is not, the ATS recommends using point at which the inspiratory volume equals 90% of the patient’s vital capacity as the end of inspiration.
Regardless of the method used to measure breath-hold time, the periods of inhalation and exhalation should be kept as short as possible in order to minimize measurement inaccuracies. The formula used to calculate DLCO does not by itself differentiate between the inhalation phase, breath-hold period and the exhalation phase; all are considered to be part of the breath-hold period. Several researchers have devised techniques that calculate and then integrate DLCO for each of these phases. This approach is based on physiological models and is known as the 3-equation method. It is available on some test systems but is not recommended by the ATS or ERS at this time.
As mentioned previously, the choice of a 10-second breath-hold period was somewhat arbitrary. In subjects with normal lungs, DLCO tends to decrease when breath-holding lasts longer than 10 seconds. A variety of potential causes for this have been proposed which include build-up of CO back pressure and changes in circulation but regardless there seems to be little reason to propose a longer breath-holding period. A shorter breath-holding period may be acceptable since at least one study has shown that breath-holding periods of 6 or 8 seconds gives reasonably equivalent results. The problem with shorter breath-holding periods is that inspiration and expiration become a significant part of the overall time period.
These findings apply primarily to subjects with normal lungs however. There is general agreement that patients with COPD show increases in DLCO with longer breath-holding times. For these patients a longer breath-hold time allows more time for axial diffusion and therefore increased ventilation of poorly ventilated lung units as well as a better estimation of VA.
It should also be remembered that the conditions under which the breath-hold period is conducted can also affect the measured DLCO. During the breath-hold period, a Valsalva maneuver (forcible exhalation against a closed airway) acts to raises the intrathoracic pressure thereby decreasing both the pulmonary blood volume and the DLCO. A Muller maneuver (forcible inhalation against a closed airway), on the other hand, decreases intrathoracic pressure, thereby increasing pulmonary blood volume and the DLCO. For these reasons the ATS-ERS Statement on DLCO testing recommends that the patient avoid excessive positive (Valsalva) or negative (Muller) pressure maneuvers during the breath-hold period. Determining whether these have occurred, however, can be difficult. Most DLCO tests system have a valve arrangement that prevents exhalation during the breath-hold period. Some of the test systems my lab uses monitor airway pressure during the breath-hold period but the usefulness of this measurement assumes the patient keeps their airway open during breath-hold and my impression is that most patients close their glottis instead.
There are many approaches towards measuring gas exchange, but the single-breath DLCO has become the primary way of making this measurement. The single-breath DLCO test is an artificial maneuver that nevertheless provides clinically significant information about gas exchange. How the BHT is measured has implications for DLCO calculations and should also be a consideration when choosing DLCO reference equations. Because the BHT includes some or all of the inspiratory and expiratory components of the maneuver it necessarily simplifies a complex situation. The Jones-Meade approach to measuring BHT attempts to minimize these components and is probably a good compromise. Although the choice of a 10 second BHT was fairly arbitrary it also appears to strike a good balance between physiology, patient abilities and test equipment limitations.
REFERENCES:
Beck KC, Offord KP, Scanlon PD. Comparison of Four Methods for Calculating Diffusing Capacity by the Single Breath Method. Chest 1994; 105:594-600
Brusasco V, Crapo R, Viegi G editors. ATS/ERS Task Force: Standardization of Lung Function Testing. Standardization of the single-breath determination of carbon monoxide uptake in the lung. Eur Resp J 2005; 26:720-735
Dressel H, Filser L, Fishcher R, de la Motte D, Steinhaeusser W, Huber RM, Nowak D, Jorres RA. Lung diffusing capacity for nitric oxide and carbon monoxide: Dependence on breath-hold time. Chest 2008; 133:1149-1154
Ferris BG, ed. Epidemiology Standardization Project. Am Rev Resp Dis 1978; 118:6(Part 2;1-120)
Graham BL, Mink JT, Cotton DJ. Overestimation of the Single-Breath Carbon Monoxide Diffusing Capacity in Patients with Air-Flow Obstruction. Am Rev Resp Dis 1984; 129:403-408
Graham BL, Mink JT, Cotton DJ. Effect of breath-hold time on DLCO(SB) in patients with airway obstruction. J Appl Physiol 1985; 58:1319-1325
Jones RS, Meade FA. Pulmonary Diffusing Capacity: an improved single-breath method. Lancet 1:94-95
Lawson WH. Effect of drugs, hypoxia and ventilatory maneuvers on lung diffusion for CO in man. J Appl Physiol 1972; 32:788
Leech JA, Martz L, Liben A, Becklake M. Diffusing Capacity for Carbon Monoxide: The Effects of Different Derivations of Breathold Time and Alveolar Volume and of Carbon Monoxide Back Pressure on Calculated Results. Am Rev Resp Dis 1985; 132:1127-1129
Ogilvie CM, Forster RE, Blakemore WS, Morton JW. A Standardized Breath Holding Technique For The Clinical Measurement Of The Diffusing Capacity Of The Lung For Carbon Monoxide. J Clin Invest 1957; 36:1-17

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.

Richard, in the regular spirometry test, the patient is encouraged to take as “deep a breath as possible.” From you descriptions, above, with regard to overestimating/underestimating, it would seem that, with the DLCO test which requires a breath-holding period of time, surely, a very forceful, deliberate effort to to fill the lungs with air would necessitate a closing of the airways in order to hold that full-capacity of air in the lungs intact for 10 seconds; and therefore an automatic tendency for the DLCO value to be underestimated.
Would it be better if the technician conducting the DLCO test instructed the patient not to inhale “as much as -possible- (as with the Spirometry test),” but rather just a “deep breath;” which could be held more easily for 10 seconds, and therefore reduce the occurrence of exhaling against a closed airway. Yes, defining “deep breath” as opposed to “as deep a breath as possible” may be difficult to achieve in practice, but a “test-run” to coach the patient into not “overdoing it” on inhalation seems doable.
Also, I’d like to ask a question about the DLCO test with regard to smokers.
From what I understand, a smokers DLCO test can be underestimated just due to the fact that at least half of all smokers will have -at least- a 5% increase above normal CO on the hemoglobin, and the DLCO value will decrease by 1% for every 1% above normal of CO on the hemoglobin.
However, given that, are there other factors peculiar to smokers that can underestimate the DLCO values? Specifically, uncleared “smokers-cough” production, which may “artificially” interfere with the Alveolar absorption process (or delay, and therefore shorten the necessary “time” needed) during the test.
In other words, would, in general, a smoker who hasn’t smoked for, say, three days before the test have a significantly higher percentage of diffusing capacity that a smoker who smoked one hour before the test?
I’ve noticed that most material on the subject recommens a 24 hour no-smoking period before the DLCO test, yet, with my own instructions before I took the test was just a 1 hour no-smoking period before the DLCO test.
Gas exchange depends on surface area and the lung’s surface area is maximum at or near TLC. For this reason a maximal inhalation is necessary and the ATS-ERS standard says that the inspired volume must be at least 85% of the largest VC. I’m also not sure that the length of time an individual can breath-hold comfortably has anything to do with how deep a breath you take beforehand. Closing your glottis (which is what I think you meant by “closing the airways”) and then bearing down (which is a Valsalva maneuver) will decrease the blood volume and blood flow in the lung and yes, will decrease DLCO. But most patients can hold their breath without bearing down and for the 10 seconds of the test this does not affect the blood flow or volume of the lung.
The ATS-ERS statement on DLCO testing says that “As cigarette smoking is the most common source of COHb, subjects should be asked to refrain from smoking or other CO exposures on the day of the test.” A recent cigarette (within an hour of a DLCO test) will dramatically increase the amount of carbon monoxide in an individual’s alveolar air as well as the carbon monoxide in their blood (and transiently decrease their DLCO) so I suppose that an hour of non-smoking is better than none. Three days is more than enough time for all of the residual carbon monoxide to disappear and this would likely improve results(maybe significantly, maybe not but that depends on how you want to define “significant”), but how likely are you to get a smoker to stop smoking that long just for a DLCO test? If you are concerned about carbon monoxide levels affecting test results a more realistic approach would be to get a blood sample, measure the COHb and correct the test results accordingly or measure the alveolar level of carbon monoxide and do the same (you can estimate COHb from PACO).
Smoker’s cough is a symptom of chronic bronchitis which is an obstructive lung disease. You could argue that when airway obstruction like this is present the inhaled DLCO test gas mixture does not get completely or evenly distributed in the lung and for this reason DLCO may be underestimated but at the same time, isn’t that a more-or-less accurate reflection of their ability to get oxygen in their blood stream? There are mechanical issues involved with the lung’s gas exchange (i.e. gas transport and gas diffusion in the terminal airways) as well as physiological (the alveolar-capillary membrane and ventilation-perfusion matching) and a DLCO test result (and real-life gas exchange) will be affected by both. Yes, you could argue that the mechanical issues should somehow be ignored in order to measure “real” gas exchange but even if that could be done, how does that show the actual clinical picture?
Thank you for the reply.
Good point about the fact that, with a smoker, whatever the conditions are (mucus plugging in the airways, etc.) at the time of the test, are that individuals “normal” breathing/blood oxygen processing situation.
However, although I haven’t seen the term “reversibility” used with DLCO testing (as it’s used so often with Spirometry and post-bronchodilator) it may also apply to DLCO in that, if the patient quits smoking, they could immediately realize a significant change for the better with regard to diffusing capacity.
How do you know if pt inhaled too early during end of exhalation (to capture CO) during dlco
J –
I’m not sure if I understand your question. During the initial exhalation to RV some test systems display the exhaled volume curve and a technician can use this to judge whether the patient has exhaled completely before taking the inhalation of the DLCO gas mixture. Not all test systems do this however and realistically you can only compare the Inspired Volume to the patient’s FVC and/or SVC to determine patient did exhale completely and it isn’t usually possible to do this until after the DLCO test has been performed. Even then, if the Inspired Volume is less than the FVC or SVC then there usually isn’t any way to tell if this is because they failed to exhale to RV or if they failed to inhale to TLC.
During the final exhalation after the breath-hold period as long as the patient exhales an adequate washout volume (nominally 0.75 L) and an adequate alveolar sample volume (again nominally 0.75 L) then it doesn’t really matter what the patient does after that. The new (2017) ERS/ATS DLCO test standard does require that the patient exhale to RV after the breath-hold period in order to calculate VA from a mass balance equation but if the patient does not exhale completely to RV and inhales too early that does not invalidate the test. During the exhalation following the breath-hold period if the patient inhales too soon and has an inadequate washout or alveolar sample volume then the DLCO may well be invalid.
– Richard