The patients whose reports I review have always been very accommodating. An issue of one kind or another catches my attention and before I know it I find several more reports that are similarly involved. Thanks to our patients I’ve had a number of reports come across my desk recently that showed a combination of restrictive and obstructive defects. This particular one may not be the best possible example but it seems to illustrate several points fairly well.
| Observed: | %Predicted: | Predicted: | |
| FVC (L): | 1.12 | 40% | 2.80 |
| FEV1 (L): | 0.75 | 35% | 2.16 |
| FEV1/FVC (%): | 67 | 86% | 78 |
| TLC (L): | 1.92 | 42% | 4.54 |
| FRC (L): | 1.18 | 48% | 2.47 |
| RV (L): | 0.76 | 44% | 1.73 |
| RV/TLC (%): | 40 | 104% | 38 |
Interpreting results like this as combined (or mixed) defects using the ATS/ERS algorithm seems relatively straightforward.
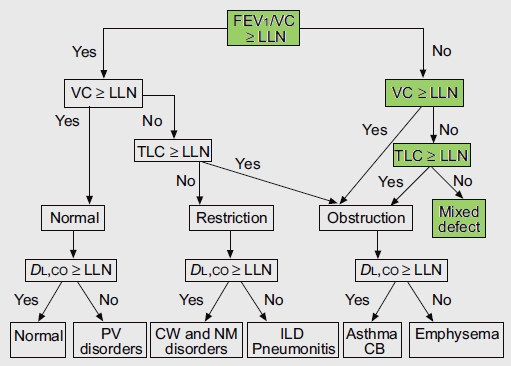
From Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standardisation of pulmonary function testing. Interpretive strategies for lung function tests. Eur Respir J 2005; 26, page 956
The algorithm starts by using the FEV1/FVC ratio to determine whether obstruction is present and only then considers whether or not the FVC and TLC are normal. It occurred to me however, that this assumes that the normal range of the FEV1/FVC ratio is preserved when TLC decreases below normal. Given the markedly different causes of restrictive lung disease it would seem that saying that the FEV1/FVC ratio should remain within the normal range over a relatively broad range of lung capacities (and without necessarily knowing the cause for any reduction) seems a bit far-fetched. Interestingly enough however, it actually turns out to be reasonably true.
In general, there are three categories of restrictive diseases; interstitial, chest wall and neuromuscular. I’ve been unable to find any studies that specifically studied the relationship between the FEV1/FVC ratio and TLC but there are numerous studies of these disorders where spirometry and lung volumes were performed.
In regards to interstitial disease, a study of over 200 patients with idiopathic pulmonary fibrosis and a reduced TLC showed that the FVC was decreased more than the FEV1 (61% vs 71%). Similarly, a study with a small number of patients with Sjogren’s disease (an autoimmune disease that can cause interstitial lung disease) showed that those individuals with a reduced TLC had an FVC that was decreased slightly more than the FEV1.
In regards to chest wall diseases, several studies on patients with ankylosing spondylitis also showed that in those individuals with a reduced TLC that the FVC decreased more than the FEV1. Finally, in regards to neuromuscular disease a study of 25 patients with ALS, the FVC was decreased slightly more than the FEV1.
This means that at least for these examples of restrictive disease the FEV1/FVC ratio is preserved and maybe even slightly elevated. Given this, it does appear that a reduced FEV1/FVC ratio in combination with a reduced TLC is a probably a reliable indicator of a mixed defect. It could even be argued that because in all of these cases the FVC decreased somewhat more than the FEV1 the lower limit of normal (LLN) for the FEV1/FVC ratio should increase when restriction is present. Since the relationship between FVC and FEV1 differs somewhat from one category of restriction to another and because the cause of restriction is often unknown making an accurate adjustment of this kind does not seem to be realistic.
Once a set of results have been interpreted as having a mixed defect however, it turns out that assigning a level of severity to the restrictive and obstructive components is more than somewhat problematic. Part of the reason for this is that the ATS/ERS standards do not include an index of severity for a reduced TLC and instead just say that a TLC below the LLN indicates restriction.
Note: The recommendation that the LLN be used to determine restriction is somewhat problematic due to the fact that most lung volume reference equations (which often come from several decade-old studies) do not include an LLN. LLN therefore must be calculated using the statistics for the entire study population which means the LLN becomes a fixed value that is subtracted from the predicted TLC regardless of an individual’s height or age. Moreover, the TLC itself is often adjusted using correction factors for ethnicity and there are no recommendations on how to adjust the LLN for this. Finally, the predicted lung volume values are also often modified by the insertion of an FVC from a different set of reference equations and this can skew the TLC away from its original reference value without any modification of the LLN. For these (and other) reasons many labs just use 80% of predicted as a cutoff instead of the LLN.
The severity index my lab uses for TLC has been handed down from generation to generation and originated at the NIH in the 1970’s. I can’t say that it is 100% correct or that it has been clinically verified but it is in common use in many PFT labs:
| TLC ≥ 80% | Normal |
| TLC ≥ 60% and <80% | Mild |
| TLC ≥ 40% and <60% | Moderate |
| TLC < 40% | Severe |
The other problem is that the ATS/ERS recommendations for the severity of airway obstruction are based solely on the FEV1 percent predicted.
| ATS: | Mild | FEV1 ≥70% predicted |
| Moderate | FEV1 ≥60% and ≤70% predicted | |
| Moderately Severe | FEV1 ≥50% and ≤60% predicted | |
| Severe | FEV1 ≥35% and ≤50% predicted | |
| Very Severe | FEV1 <35% predicted |
In a mixed defect however, the FEV1 is reduced not just because of obstruction but because of restriction as well. At least two different approaches towards correcting this have been suggested.
Balfe et al proposed using the FEV1/FVC ratio to assess severity. This approach was originally a recommendation from the Intermountain Thoracic Society’s 1984 manual. Specifically the FEV1/FVC ratio’s confidence interval (1.65 times the standard error of the estimate) is used to derive an index of obstruction severity.
| ITS: | Mild | FEV1/FVC reduced by ≥1 and <2 CI |
| Moderate | FEV1/FVC reduced by ≥2 and <4 CI | |
| Severe | FEV1/FVC reduced by >4 CI |
Balfe et al showed that when the FEV1 percent predicted was used, over 90% of the patients with mixed defects were interpreted as having severe obstruction. When the FEV1/FVC ratio was used over 90% of the same patients were instead interpreted has having mild or moderate obstruction. Using the FEV1/FVC ratio from the mixed report above, the level of obstruction would be changed from severe to mild. To some extent this seems to be a reasonable approach, but is limited by the dependence of the FEV1/FVC ratio on the FVC and the quality of the expiratory effort.
Gardner et al on the other hand, proposed adjusting the FEV1 percent predicted using the TLC percent predicted. Specifically, the percent predicted FEV1 is divided by the TLC percent predicted and then the ATS/ERs criteria are used. For example, using the results from the mixed report above:
35% predicted/42% predicted = 0.83 or 83% predicted
which also changes the severity from severe to mild. Similar to Balfe et al, this approach reduced the assessed severity of 83% of the patients in a study group of 199 patients This approach also seems to be reasonable and has the advantage that it is independent from the FVC and FEV1/FVC ratio. The one criticism I would make of Gardner et al’s proposal is that the reference equations for FEV1 and TLC are derived from different populations and the effect that different reference equations than those selected for the study would have on the correction factor was not studied.
An observation made by several different investigators is that when restriction and obstruction are both present, the RV should be elevated and in fact the absence of an elevated RV was used to exclude patients from a study population in one or two instances. The point is that an elevated RV is a sign of obstructive hyperinflation and should be present in a mixed defect. It’s not clear to me however, that an elevated RV should always be present in a mixed defect, particularly given the different causes of restriction and particularly when the obstruction is “mild”. There is also the fact that an elevated RV can be due in part or in whole to a suboptimal SVC maneuver. For these reasons it would seem that an elevated RV shouldn’t be a required feature in the interpretation of a mixed defect.
One final point is that when restriction is relatively severe the amount by which a decrease in FEV1 will cause a coexisting obstructive defect to be observed becomes quite small. In the report presented above, if the FVC was actually normal the FEV1 would need to decrease by 0.30 L from its predicted value for the FEV1/FVC ratio to be 86% of predicted. In this case however, when the FVC is 40% of predicted the FEV1 only needs to be 0.11 L less than it “should” be for the FEV1/FVC ratio to be 86% of predicted. This volume is less than the required repeatability for the FVC and FEV1 (0.15 L). Since individuals with this degree of restriction are often debilitated the quality of the FEV1 (and FVC) should be carefully considered before the interpretation of a mixed defect is made.
Mixed defects, where both restriction and obstruction are present at the same time, are relatively rare. In one study with a general population of 7506 patients that had both lung volumes and spirometry performed only 151 patients (2%) satisfied the criteria for a mixed defect. The FEV1/FVC ratio is a critical component in diagnosing mixed defects and appears to remain within normal limits both within the different categories of restrictive lung disease and over a broad range of lung volumes.
Assigning severity to the restrictive and obstructive components of a mixed defect remains problematic due to limitations in the current ATS/ERS standards. Using the ATS/ERS standard for obstructive severity based on the FEV1 percent predicted appears to significantly overestimate the actual level of severity in mixed defects. At least two different proposals have been made to correct this problem and both have similar effects on the assigned severity. As always, test quality is important and the diagnosis of a mixed defect should neither be made nor should it be excluded when test quality is lacking.
References:
Balfe DL, Lewis M, Mohsenifar Z. Grading the severity of obstruction in the presence of a restrictive ventilatory defect. Chest 2002; 122: 1365-1369.
Berdal G, Halvorsen S, van der Heijde D, Mowe M, Dagfinrud H. Restrictive pulmonary function is more prevalent in patients with ankylosing spondylitis than in matched population controls and is associated with impaired spinal mobility: a comparative study. Arthritis Research & Therapy 2012; 14: R19
Brusasco V, Crapo R, Viegi G. ATS/ERS Task Force: Standardisation of pulmonary function testing. Interpretive strategies for lung function tests. Eur Respir J 2005; 26: 948-968.
Culver BH. Obstructive? Restrictive? Or ventilatory impairment? Chest 2011; 140: 568-569
Gardner ZS, Ruppel GL, Kaminsky DA. Grading the severity of obstruction in mixed obstructive-restrictive lung disease. Chest 2011; 140: 598-603.
Grimby G, Fugl-Meyer AR, Blomstrand A. Partitioning of the contributions of rib cage and abdomen to ventilation in ankylosing spondylitis. Thorax 1974; 29: 179-184.
Diaz-Guzman E, McCarthy K, Stoller JK. Frequency and causes of combined obstruction and restriction identified in pulmonary function tests in adults. Respir Care 2010; 55(3): 310-316.
King TE, Tooze JA, Schwarz MI, Brown KR, Cherniak RM. Predicting survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 2001; 164: 1171-1181.
Lechtzin N, Wiener CM, Shade DM, Clawson L, Diette GB. Spirometry in the supine position i
Lanier RC, Olsen GN. Can concomitant restriction be detected in adult men with airflow obstruction? Chest 1991; 99: 826-830
Segal I, Fink G, Machtey I, Gura V, Spitzer SA. Pulmonary function abnormalaties in Sjogren’s syndrome and the sicca complex. Thorax 1981; 36: 286-289.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License
