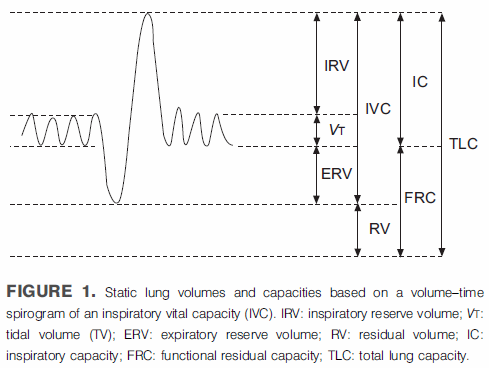
The plethysmographic technique for measuring lung volumes determines FRC first and then uses a slow vital capacity maneuver to calculate TLC and RV. FRC is defined as the volume of the lung at the end of a normal exhalation. The two components of the SVC maneuver that are used to calculate TLC and RV are the Inspiratory Capacity (IC) and the Expiratory Reserve Volume (ERV) and they too are measured relative to FRC. It would therefore seem to be important to have an accurate notion as to where FRC is in relation to TLC and RV when measuring lung volumes.
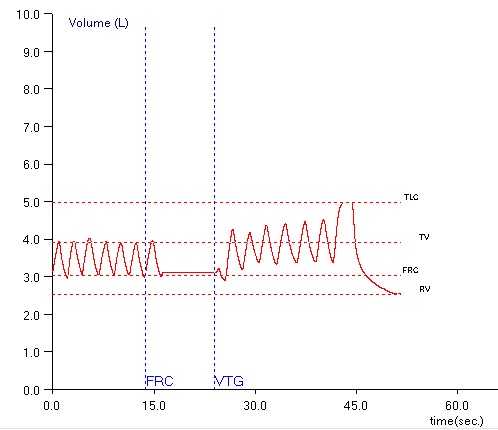
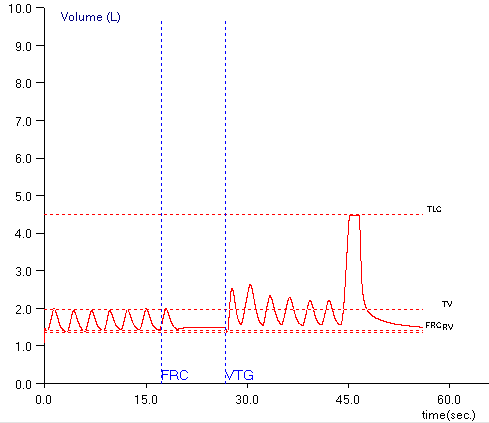
Plethysmography measures lung volumes by having a patient pant against a closed shutter and measuring pressure changes. The test is usually performed by having the patient breathe tidally for a period in order to determine where end-exhalation (FRC) is located, closing the shutter and performing the measurement, then returning to tidal breathing and performing the SVC maneuver. A critical assumption in this process is that the FRC baseline does not change while the shutter is closed.
Patients are incredibly ingenious, however, and often find a way to shift their FRC baseline during plethysmography. This is often due to a leak of some kind and when this occurs, both TLC and RV can be mis-estimated.
If the baseline shifts upwards, then TLC and RV will both be overestimated.
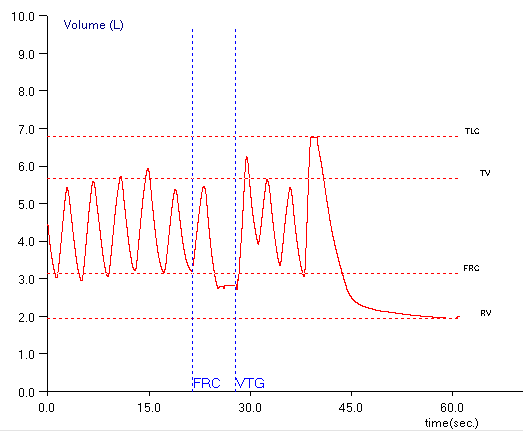
If the baseline shifts downwards, then TLC and RV will both be underestimated.
This is something that “everybody” knows about and is documented to some extent in the ATS-ERS guidelines and our manuals for the test equipment. At the moment, the software used in my PFT Lab does not allow us to correct for FRC baseline shifts so technicians are taught to recognize when a significant baseline shift has occurred and to not use the results from that test.
When FRC baseline shifts occur then as the last two examples show it is often quite evident and easy to recognize, but just as often it is much less clear less clear that a baseline shift has occurred and if it has, whether it is significant or not. Closing the shutter often affects how patient breathe and they may shift their baseline for this reason and not because they leaked. Eventually they may return to their original baseline, but in this example is this what happened or not?
Since shutter closure can affect a patient’s breathing pattern and FRC, if they drift off baseline after the shutter has re-opened is it because a change in lung mechanics or did they leak and are actually returning to their “real” FRC?
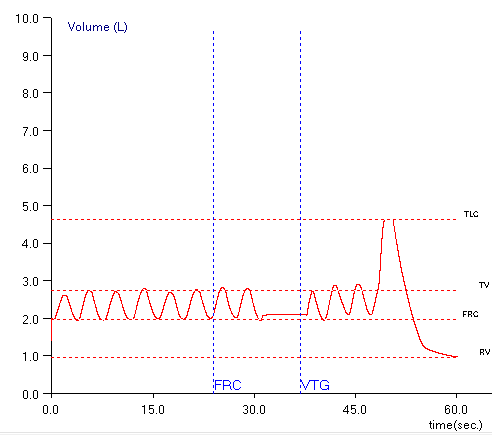
Finally, what is a significant change in FRC baseline? I’d rather only report the results from tests that had no baseline shift but you often have to work with what you can get. That makes this an important question and there does not appear to be a clear answer. The ATS-ERS guidelines recommend that to be reported serial measurements of FRC by plethysmograph should differ than no more than 5 percent. FRC baseline shifts however, do not affect the measurement of FRC, but of TLC and RV. 5 percent, however is probably a reasonable value to apply to TLC. Does that mean that a baseline shift less than 5% of TLC is acceptable?
The baseline shift in this example is approximately 0.16 L, which is 3.5% of the TLC and probably acceptable, particularly if it is the best you can get from a patient, but since there are no guidelines this is a guess. I’d also have to mention that estimating the error is also problematic because the best you can do within the test module is eyeball the graph and guestimate the volume shift (I was able to use a graphics program and apply a tape measure but that was a separate program and required a screen dump).
At a very rough estimate I’d say that about half of our plethysmographic lung volume measurements do not have any baseline shifts. Although the ATS-ERS guidelines ask for three acceptable quality tests with repeatable FRC measurements the reality is that we have to work with imperfect test results and for a variety of reasons there is a certain fraction of patients that just don’t seem to be able to perform plethysmography correctly.
I have to ask why the post-shutter FRC is not re-assessed by our lab’s testing software. It seems to me that it would be relatively simple to check a patient’s end-exhalation level both before and after shutter closure and to show any discrepancy between the two measurements. I would also appreciate the ability to “fix” TLC and RV calculations that have been incorrectly calculated from mis-estimated IC and ERV measurements caused by a FRC baseline shift. Finally I’d like to see the ATS-ERS guidelines have a better appreciation of potential testing errors from all lung volume measurement techniques with a consensus about what level of error is acceptable.
Plethysmography is still considered by many to be the gold standard in lung volume measurement. There are a number of reasons, FRC baseline shifts being one of them, that plethysmography cannot be considered to be any more accurate than helium dilution or nitrogen washout lung volumes. I am concerned that many of the possible error modes in plethysmography (and helium dilution and nitrogen washout) are not as well appreciated as they should be and that all too often results are accepted because “the computer said they were okay”.
References:
Brusasco V, Crapo R, Viegi G. Standardisation of the measurement of lung volumes. Eur Respir J 2005; 26: 511-522.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.