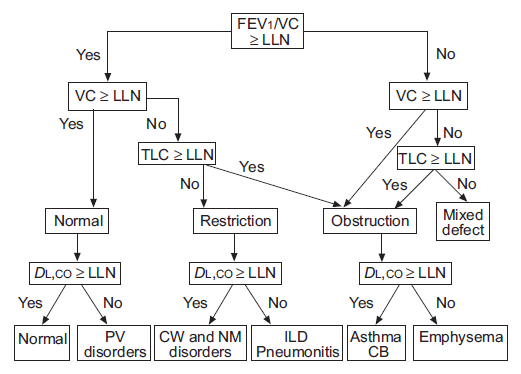
A low FEV1/VC ratio is the primary indication for airway obstruction.
The ATS/ERS statement on interpretation says
“The VC, FEV1, FEV1/VC ratio and TLC are the basic parameters used to properly interpret lung function (fig. 2). Although FVC is often used in place of VC, it is preferable to use the largest available VC, whether obtained on inspiration (IVC), slow expiration (SVC) or forced expiration (i.e. FVC).”
I understand and in general agree with the idea of using the largest VC regardless of where it comes from and this is because the FVC is often underestimated for any number of good (and not so good) reasons. When this happens the FEV1/FVC ratio will be overestimated and airway obstruction will be under-diagnosed. However the ATS/ERS statement is also grounded in the notion that all vital capacities (FVC, SVC, IVC) are the same and this isn’t necessarily true. The problem comes from the fact that the predicted values and lower limit of normal (LLN) for the FEV1/VC ratio always come from reference equations for FEV1/FVC ratios. Because the SVC (and IVC) are usually larger than the FVC this means there is at least the potential for airway obstruction to be over-diagnosed.
An FVC maneuver is designed to measure the maximum expiratory flow rates, in particular the FEV1 and the PEF. It has long been recognized that the effort involved in the FVC maneuver can cause early airway closure, even in individuals with normal lungs, and that for this reason the vital capacity can be underestimated due to gas trapping. This effect is usually magnified with increasing age and in individuals with obstructive lung disease. Moreover, it is universally acknowledged that the FVC maneuver can be a stressful maneuver for many patients and there are a number of good reasons why an expiration should be terminated before the maximum possible vital capacity has been exhaled.
An SVC maneuver is designed to measure the lung volume subdivisions, Inspiratory Capacity (IC) and Expiratory Reserve Volume (ERV), and to maximize the measured volume of the vital capacity. Due to the more relaxed nature of the SVC maneuver there is significantly less airway closure and for this reason the SVC volume is usually larger than the FVC, even in individuals with normal lungs.
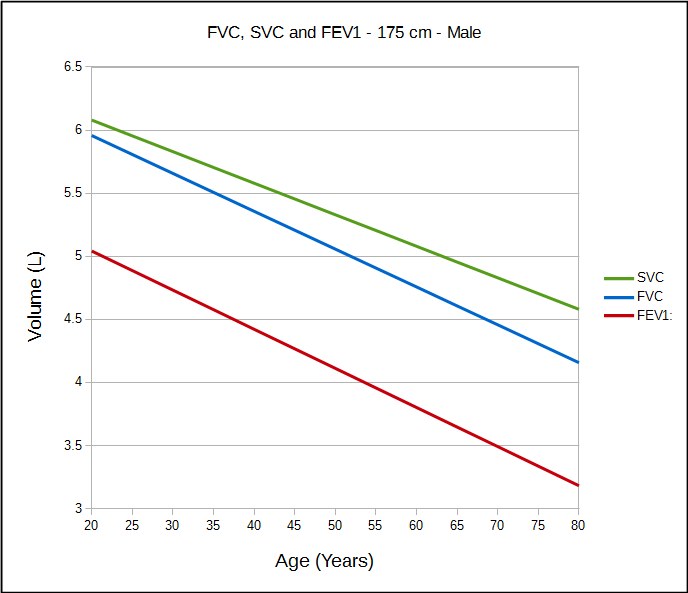
There are very few studies that have derived reference equations for FVC, SVC and FEV1 from the same population., but those from Marsh et al make the differences between FVC and SVC relatively clear.
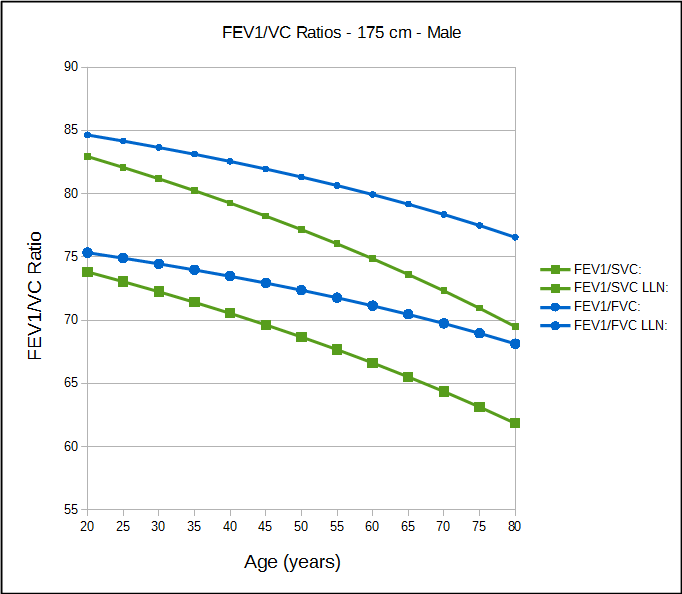
Because the SVC is usually larger than the FVC, the FEV1/SVC ratio will usually be lower than the FEV1/FVC ratio. Although Marsh et al derived a reference equation specifically for the FEV1/FVC ratio they did not do the same for the FEV1/SVC ratio. For this reason, I’ve calculated a predicted FEV1/FVC ratio from the individual reference equations for FVC and FEV1, and then a predicted FEV1/SVC ratio from the individual reference for SVC and FEV1 (this may well be mis-using the reference equations but I’m trying to show comparable values). For an LLN I’ve used the LLN from the NHANES III reference equations, which is approximately 89%.
What this shows is that a normal FEV1/SVC ratio is lower than the FEV1/FVC ratio for all ages and that the difference increases with increasing age. This also means that a spirometry effort with a normal FEV1/FVC ratio will sometimes be considered abnormal when an SVC is used to calculate the FEV1/VC ratio.
Is this really a problem?
On the one hand, I’d say that the FVC is often underestimated and that the SVC is probably a better indication of a patient’s VC than the FVC. On the other hand I’ve seen FVC efforts with a normal FEV1/FVC ratio that met (or exceeded) all ATS/ERS criteria for test quality but where the SVC was sufficiently larger than the FVC that the FEV1/SVC ratio showed mild airway obstruction.
Since the ATS/ERS statement on interpretation does not acknowledge that there is any difference between an FVC and an SVC there are no particular guidelines for assessing whether or not a reduced FEV1/SVC by itself is a reliable indicator of airway obstruction. In fact, since this topic does not appear in any literature searches and none of the textbooks I have discuss it (other than to say to follow the ATS/ERS guidelines) there does not appear to be any guidelines on this issue whatsoever.
I think this has to be decided on a case-by-case basis and that this issue rests first and foremost on the quality of the FVC measurement. Whenever there is any reason to believe the FVC may be underestimated, and this can be the case even when the ATS/ERS criteria are met, then there is no reason not to the believe what the FEV1/SVC ratio is saying. For all other cases, particularly when it is only the FEV1/SVC ratio that is below the LLN, this leaves any diagnosis of airway obstruction in a somewhat gray area.
Any certainty that a reduced FEV1/SVC ratio indicates airway obstruction is present has to depend at least in part on how far it is below the FEV1/FVC LLN. A good question however, is how far below it needs to be. Since the discrepancy between FVC and SVC increases with age, I would be more likely to believe that a reduced FEV1/SVC ratio indicates airway obstruction in a young individual than in one that was elderly. The reference equations from Marsh et al indicate that the FEV1/SVC LLN is approximately 2 percentage points below the FEV1/FVC LLN at age 20 and approximately 8 percentage points at age 80. Marsh et al is only a single study however, and to be honest it was chosen as an example because it showed a reasonably clear difference between FVC and SVC at all ages. Another study (Gutierrez et al) also has reference equations for FVC, SVC and FEV1 derived from the same population but shows a much smaller difference in FVC, SVC, FEV1/FVC and FEV1/SVC over the same age range.
Note: On a related issue, it’s one thing to knowingly compare the FEV1/FVC and FEV1/SVC ratios, but I’ve seen lab software that automatically substituted the SVC for the FVC (and vice versa) without any indication this has happened (i.e. the report still said FVC, FEV1/FVC and SVC despite them having been interchanged). I don’t necessarily have a problem with software automatically substituting an SVC for an FVC (although I do with vice versa) but I’d want to know this had happened.
We seem to have an interesting blind spot about the FVC and the SVC being the same when it is easy to demonstrate that they are not. When it comes to routine clinical spirometry however, the FVC is frequently underestimated and an SVC (or an IVC) is likely a better indication of a patient’s VC. The problem is that in these cases we are assessing the presence of airway obstruction using the FEV1/SVC ratio but with reference equations and LLN’s for the FEV1/FVC ratio. The number of individual’s that are mis-diagnosed by a reduced FEV1/SVC ratio is probably small, but it more likely occurs in the elderly than in the young, and since it has never been studied the false-positive rate is unknown.
In a sense, the crux of the matter is that the FEV1/FVC ratio depends on both the FEV1 and FVC. Even when the ATS/ERS criteria are met we can’t ever be 100% certain we’ve measured a patient’s maximum VC (and this is one of the arguments in favor of the FEV6 and FEV1/FEV6 ratio). At best we can only approximate it. Given that the FEV1/VC ratio depends on one measurement that requires maximum expiratory flow (FEV1) and one that requires maximum volume (VC), it would seem that the maneuvers needed to achieve these values should probably be different. Until such time as the standards for routine spirometry change to include separate FEV1 and VC maneuvers however, and that the reference equations reflect this, the best we can do is to keep the differences between FVC and SVC in mind when reviewing test results.
References:
Brusasco V, Crapo R, Viegi G. ATS/ERS task force: Standardisation of lung function testing. Interpretive strategies for lung function tests. Eur Respir J 2005; 26: 946-968.
Gutierrez C, et al. Reference values of pulmonary function tests for Canadian caucasians. Can Respir J 2004; 6: 414-424.
Marsh S, Aldington S, Williams M, Weatherall M, Shirtcliffe P, McNaughton A, Pritchard A, Beaseley R. Complete reference ranges for pulmonary function tests from a single New Zealand population. New Zealand Med J 2006; 119: N1244.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License

one thing i’m curious about is that I’ve made several comments here, some I thought were relevant to the conversation. I have as much experience as the blog author, been department head in some large institutions and had peer reviewed articles. Yet, not one of my comments have made it to the final version.
Any reason why?
Mike –
If you posted a comment and it didn’t appear within a day then it probably got misdirected by this website’s spam filter. I get a couple hundred spam comments a week, sometimes more, and rely on a service called Akismet and it’s Spam filter. So far the filter seems to work well and you are the first to complain about comments going astray. If you, or anybody else, posts a comment and it doesn’t show up on the website in less than a day please email me and I will try to retrieve it from the Spam filter. I always welcome comments, even if I don’t agree with them, and will never edit them or prevent them from being posted.
Regards, Richard
Hi. The following study to be presented at the next ERS meeting in London (2016) asked exactly the question you nicely poised…a very challenging topic indeed!
Usefulness of FEV1/SVC to uncover airflow obstruction in subjects with preserved FEV1/FVC
Saint-Pierre M, Ladha J, Berton DC, Zapotichny A, Faubert D, Crozier-Wells L, Tang J, Muir C, Forkert L, O’Donnell DE, Neder JA
Department of Medicine, Division of Respirology, Queen’s University, Kingston, Ontatio, Canada and Pulmonary Function Laboratory, Hotel Dieu Hospital, Kingston, Ontario, Canada.
Background: Forced vital capacity (FVC) may substantially underestimate slow expiratory VC (SVC) in patients with airflow obstruction thereby leading to a “pseudo-normal” FEV1/FVC (i.e., ≥ 0.7 and/or ≥ lower limit of normality (LLN)). It remains unclear in which specific circumstances FEV1/SVC would be helpful to uncover airway obstruction despite preserved FEV1/FVC. Methods: 15,801 consecutive spirometric measurements showing pre-bronchodilator FEV1/SVC < 0.7 and/or <LLN. Results: Twenty percent (3,031/15,801) of subjects with FEV1/SVC < 0.7 had FEV1/FVC ≥ 0.7. Among those presenting with both ratios < 0.7, 51.8% had FEV1/SVC < LLN but FEV1/FVC ≥ LLN. Most patients diagnosed with airflow obstruction only by FEV1/SVC had mild disease. However, they did present with lower FEF25-75%, higher residual volume and higher specific airway resistance than those with preserved FEV1/FVC (p<0.01). Prevalence of airflow obstruction diagnosed only by FEV1/SVC increased markedly as a function of body mass index (BMI) (e.g., 11.9% in subjects with BMI 40 kg/m2; p<0.05)). In fact, logistic regression analysis revealed that age 30 kg/m2 (2.04 (1.88-2.21)) and FEV1 > 75% predicted (1.21 (1.10-1.32)) were associated with airflow obstruction diagnosed only by FEV1/SVC (p<0.001). Conclusion: Compared to FVC, SVC increases the sensitivity of spirometry to detect mild airflow obstruction regardless the defining criterion (<0.7 or <LLN). Slow VC maneuvers are particularly helpful to uncover airflow obstruction in younger and obese subjects with largely preserved FEV1.