Most of the COPD patients that are seen in my lab tend to have little change in their FEV1 from visit to visit but their FVC often changes significantly. A change in FVC is usually related to how long a patient is able to exhale and this in turn is usually related to how well they are feeling at the time. This would seem to imply that a significant change in FVC, particularly for a patient with COPD, is, if not clinically significant, at least clinically important even when the FEV1 hasn’t changed.
The problem with this is that expiratory time can be affected by things other than how the patient is feeling. Dyspnea and fatigue, of course. As importantly some technicians are better at motivating patients than other technicians so it can also be related to which technician is performing their tests. Even when the same technician is involved however, there is no guarantee that the level of motivation or a patient’s response to that motivation will be the same.
So how do you know if a change in FVC clinically significant or not?
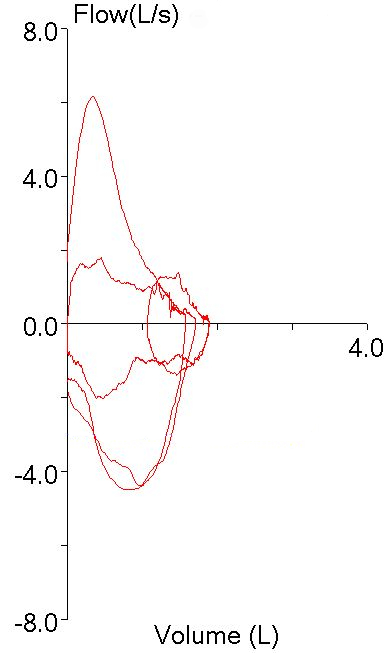
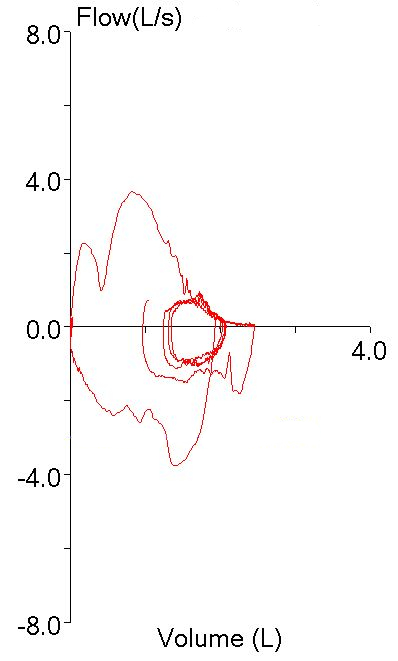
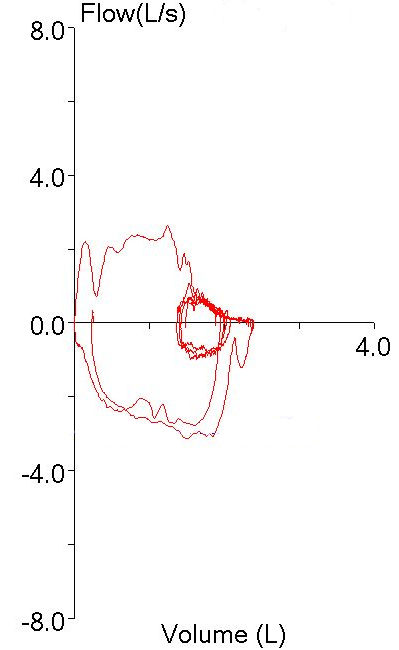
Recently a spirometry report from a patient with very severe COPD came across my desk. When comparing the results to those of the last visit I could see that there had been a small (but not significant) increase in FEV1 but at the same time there had been a large (and significant) increase in FVC.
| Visit 1: |
Observed: |
%Predicted: |
| FVC (L): |
1.28 |
36% |
| FEV1(L): |
0.53 |
19% |
| FEV1/FVC: |
41 |
53% |
| Visit 2: |
Observed: |
%Predicted: |
| FVC (L): |
1.93 |
55% |
| FEV1(L): |
0.60 |
22% |
| FEV1/FVC: |
31 |
40% |
Continue reading →