Recently a report came across my desk from a patient being seen in the Tracheomalacia Clinic. The clinic is jointly operated by Cardio-Thoracic Surgery and Interventional Pulmonology and among other things they stent airways. The patient had been stented several months ago and this was a follow-up visit. Given this I expected to see an improvement in spirometry, which had happened (not a given, BTW, some people’s airways do not tolerate stenting), but what I didn’t expect to see was a significant improvement in lung volumes and DLCO.
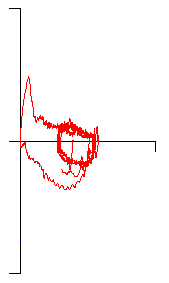
When I took a close look at the results however, it wasn’t clear to me that there really had been a change. Here’s the results from several months ago:
| Observed: | %Predicted: | Predicted: | |
| FVC: | 1.19 | 50% | 2.38 |
| FEV1: | 0.64 | 35% | 1.79 |
| FEV1/FVC: | 53 | 71% | 76 |
| TLC: | 3.21 | 76% | 4.22 |
| FRC: | 2.34 | 96% | 2.43 |
| RV: | 2.11 | 113% | 1.85 |
| RV/TLC: | 66 | 150% | 44 |
| SVC: | 1.15 | 48% | 2.37 |
| IC: | 0.87 | 48% | 1.80 |
| ERV: | 0.25 | 41% | 0.58 |
| DLCO: | 6.59 | 38% | 16.18 |
| VA: | 1.78 | 43% | 4.12 |
| IVC: | 1.04 |
[more]
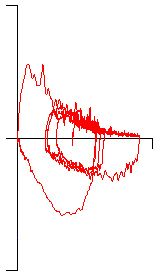
And here’s the most recent results (the slight change in predicted values is because the patient had a birthday in-between tests):
| Observed: | %Predicted: | Predicted: | |
| FVC: | 1.83 | 78% | 2.35 |
| FEV1: | 1.00 | 57% | 1.76 |
| FEV1/FVC: | 55 | 72% | 76 |
| TLC: | 3.80 | 90% | 4.21 |
| FRC: | 2.48 | 102% | 2.43 |
| RV: | 1.99 | 106% | 1.85 |
| RV/TLC: | 52 | 118% | 44 |
| SVC: | 1.82 | 78% | 2.35 |
| IC: | 1.33 | 75% | 1.78 |
| ERV: | 0.49 | 87% | 0.57 |
| DLCO: | 13.08 | 81% | 16.06 |
| VA: | 3.15 | 77% | 4.10 |
| IVC: | 1.79 |
Although the change in DLCO is impressive (+6.50 ml/min/mmHg, +99%), the baseline DLCO was actually a very marginal test. The inspired volume was only a bit over a liter (and also somewhat less than the FVC), and this is barely enough for an adequate washout and alveolar sample. More importantly the patient’s severe airway obstruction (the FEV1 was 35% of predicted) likely meant there was poor gas mixing inside their lung. This is evident from the fact that the VA is only 55% of the TLC.
The most recent test however, had an inspired volume (IVC) that was 72% higher (1.78 L vs 1.04 L) and a VA that was 77% higher (3.15 L vs 1.78 L). Since calculated DLCO scales linearly with VA (assuming that the exhaled CO and tracer gas concentrations remain the same) if the baseline DLCO had the same VA as the most recent DLCO then the DLCO would have been 11.68 ml/min/mmHg and that’s within the same ballpark as the most recent DLCO.
Even after correcting for VA I wouldn’t necessarily expect the two DLCO tests to be the same and this is because the inhaled DLCO gas mixture is not distributed homogeneously throughout the lung. In particular the low IVC in the baseline test means that only some compartments of the lung actually received the DLCO gas mixture at that time. Even so, the corrected baseline DLCO and the most recent DLCO are close enough that I have to think that despite the apparent improvement there has actually been little change in the patient’s DLCO.
The improvement in TLC isn’t as impressive (+0.69 L, +22%) but the baseline test shows an apparent restrictive defect while the most recent results are normal. There was, however, very little change in FRC (2.34 vs 2.48) and all lung volume tests (and that includes helium dilution, nitrogen washout and plethysmography) start by measuring FRC. TLC and RV are then derived from FRC using the Inspiratory Capacity (IC) and Expiratory Reserve Volume (ERV) from the Slow Vital Capacity (SVC) maneuver.
In general you might expect that when a patient becomes less obstructed that this would improve their ability to exhale more. Assuming that the FRC remains the same they would therefore have a larger ERV. That is true to some extent here since ERV does improve, but the IC improved even more and you’d expect this mostly if the FRC changed as well. Since it hadn’t this got me curious (well, more curious than I was already) so I took a look at the raw data for the baseline lung volumes (performed by plethysmography). When I did I saw that the patient had made a single acceptable effort out of six tries and the reported lung volumes were from that single effort. When I looked at the raw data for the more recent lung volumes (also plethysmography) I saw the patient had made three acceptable efforts out of four tries and that the reported lung volumes were an average of these three efforts.
FRC often changes a bit from test to test. Since the IC and ERV also change along with it (assuming you have good quality SVC efforts) this is unimportant since TLC and RV will tend to remain the same. In this case however, a single FRC measurement was being compared to an average of three measurements. IC measurements are usually the most reliable part of an SVC maneuver since a maximal inhalation is easier than is a maximal exhalation. Given the fact that the baseline FRC came from a single measurement and that the patient had been having problems performing the test in the first place, I am willing to assume that the baseline FRC was underestimated and that the improvement in TLC comes from both an increase in test quality and an increase in IC.
Post-stent the patient had a significant improvement in spirometry, but also appeared to have notable improvements in lung volumes and DLCO. I am fairly certain however, that the lung volumes and DLCO improved not because of the stent or any underlying improvement in lung function, but because of an improvement in vital capacity and test quality.
This is a reminder that not all increases or decreases in pulmonary function test results from visit to visit are real. Small changes in test quality can cause large changes in test results. I’d could say that it’s also a reminder that test quality matters but we already know that and the problem is that all too often we have to make do with whatever we’re able to get from our patients. The key however, is that anybody reviewing tests needs to understand the effect that factors like the IVC has on DLCO and the IC has on TLC and to be willing to look at more than just what’s on the surface of the report.

PFT Blog by Richard Johnston is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License