Outside the pulmonary lab there is this notion that spirometry is supposed to be so easy that anyone can do it. You just tell the patient to take a deep breath in and blow out fast and to keep blowing until they’re empty. What’s so hard about that?
Sheesh. GIGO. I keep finding ways in which the patient, their physiology and our equipment can conspire in ways to produce errors that even experienced technicians can miss. I’ve been paying a lot of attention to flow-volume loops lately and maybe it’s for this reason that I’ve seen a steady stream of spirometry tests that have something wrong with the FVC volume.
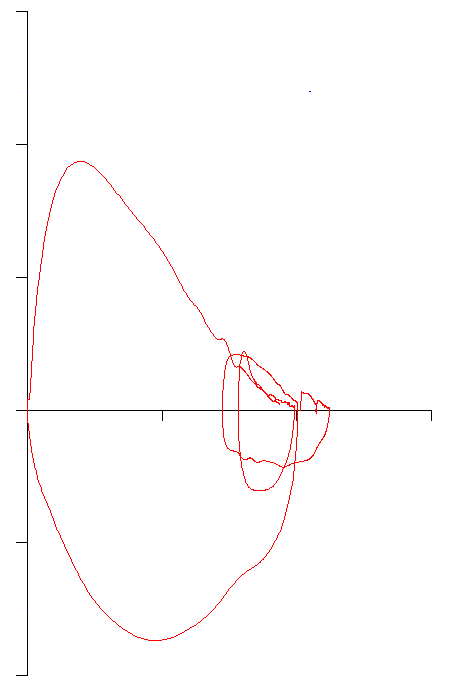
What I’ve been seeing are flow-volume loops where the end of exhalation is to the left of either the start of the FVC inhalation or of the tidal loop. Taken at face value this means that the patient did not exhale as much as they inhaled (and that the FVC is therefore underestimated) but there are several reasons why this happens and it takes a bit of detective work to figure out the cause and what to do about it.
The simplest reason is a short expiratory time. Flow-volume loops however, do not show time, only flow and volume. Sometimes when a patient stops exhaling abruptly it’s easy to see that the effort is short.
Other times it isn’t as clear:
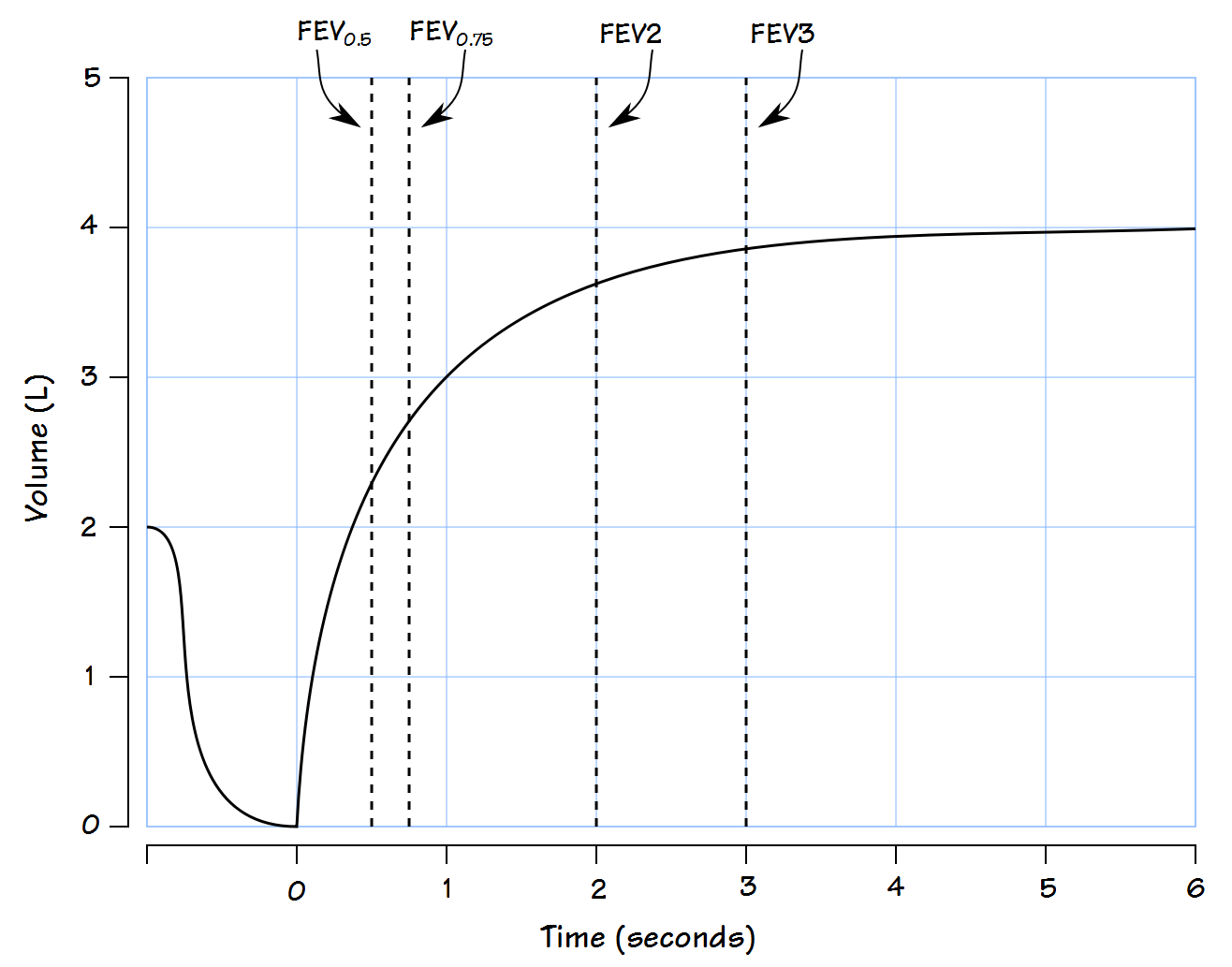
and you need to look at the volume-time curve as well.