When assessing the response to bronchodilators the change in FEV1 is used far more frequently than any other spirometry result. Other values such as inspiratory capacity (IC) and peak inspiratory flow (PIF) have also been proposed as indicators, but the ATS/ERS standards includes changes in FVC as well as changes in FEV1 and this is often overlooked. Specifically they:
“…recommend using the per cent change from baseline and absolute changes in FEV1 and/or FVC in an individual subject to identify a positive bronchodilator response. Values >12% and 200 mL compared with baseline during a single testing session suggest a ‘‘significant’’ bronchodilatation.”
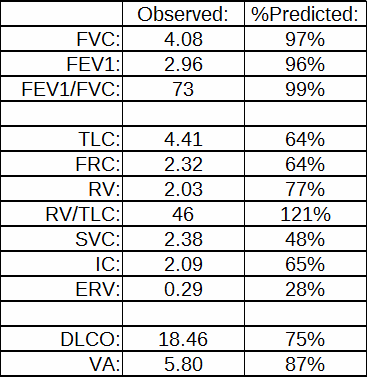
I don’t have any particular disagreement with this since post-BD increases in FVC are probably similar in nature to the post-BD changes in IC seen in some individuals with COPD. So when spirometry results like this:
| Pre-BD: | %Predicted: | Post-BD: | %Change: | |
| FVC: | 1.82 | 66% | 2.55 | +40% |
| FEV1: | 0.66 | 32% | 0.72 | +10% |
| FEV1/FVC: | 37 | 49% | 29 | -22% |
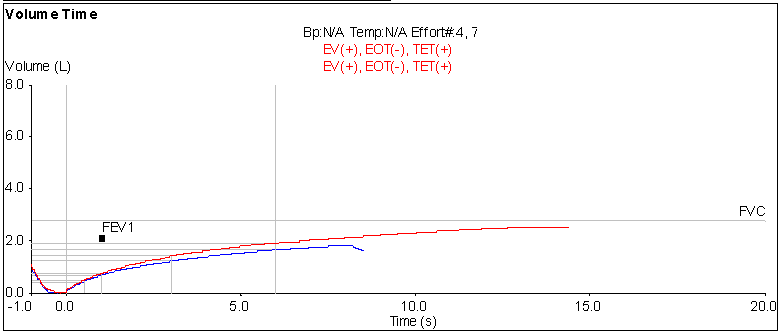
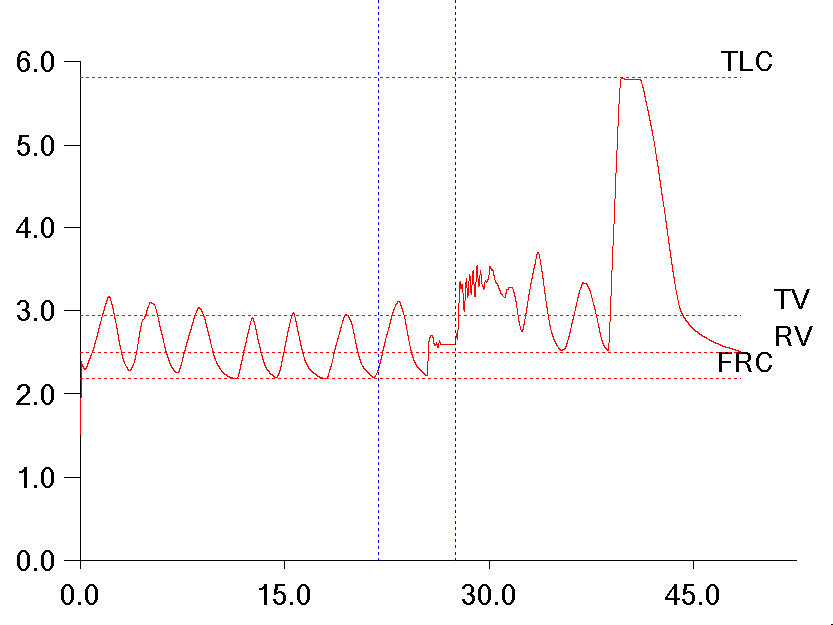
comes across my desk, I’m inclined to consider that the results show a positive bronchodilator response. Post-BD increases in FVC are not usually quite as large as 40% however, so I took a closer look at this particular test. When I did what I saw was that the post-BD test length was significantly longer than the pre-BD test length.