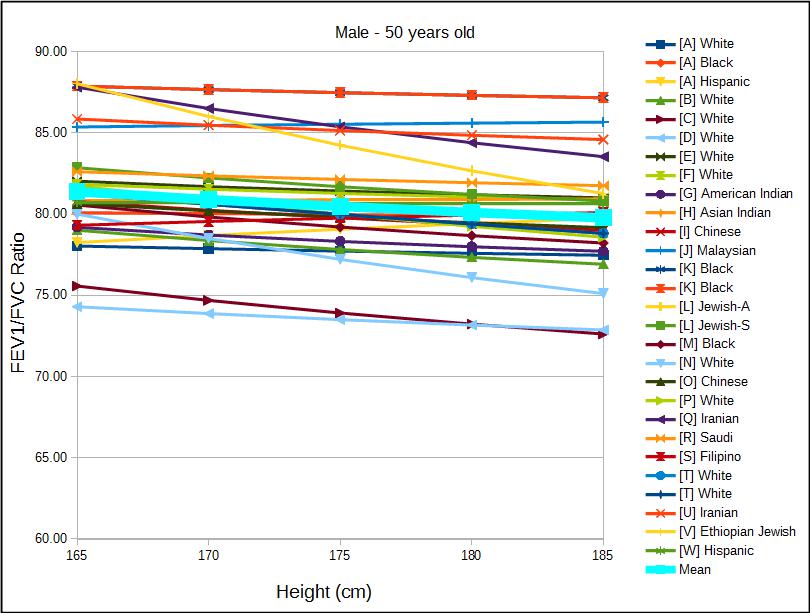
I was reading James Hansen’s textbook on pulmonary function testing and ran across a spot where he made a minor criticism of the NHANESIII (Hankinson et al) reference equations for the FEV1/FVC ratio. Specifically he noted that the NHANESIII equation ignored height and only used age as a variable but that when he compared the directly calculated FEV1/FVC ratio with one indirectly derived from predicted FEV1 and FVC there was a discrepancy across the normal ranges of height of up to 2.4%.
I had also noticed this discrepancy and wrote about it a while back but at the time I’d only been discussing my lab’s adoption of the NHANESIII reference equations. Hansen’s observation intrigued me, so I decided to re-visit this issue more systematically.
To do this I’ve taken 23 different reference equations for men and women and a variety of ethnicities and plotted the change in the FEV1/FVC ratio versus height, and then repeated this across a range of ages.