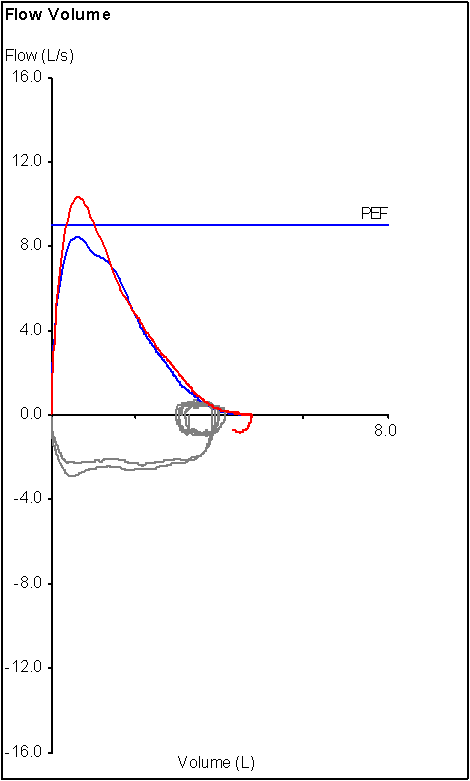
Recently I was discussing a flow-volume loop with one of our pulmonary physicians. His concern was whether the loop, which was from a patient with a cracked hyoid, was showing inspiratory obstruction or not. I had to point out that the inspiratory flows on the loop in question came from the pre-FVC inspiration that started at FRC, not RV, and that we don’t emphasize maximal inspiratory flow at that point in the test, just maximal inspiratory volume and for these reasons the flow-volume loop was not a reliable indicator of inspiratory obstruction.
Monthly Archives: October 2014
When a Pulmonary Mechanical Limitation to exercise isn’t the real limitation
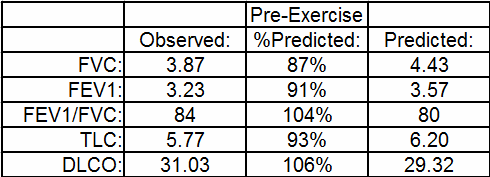
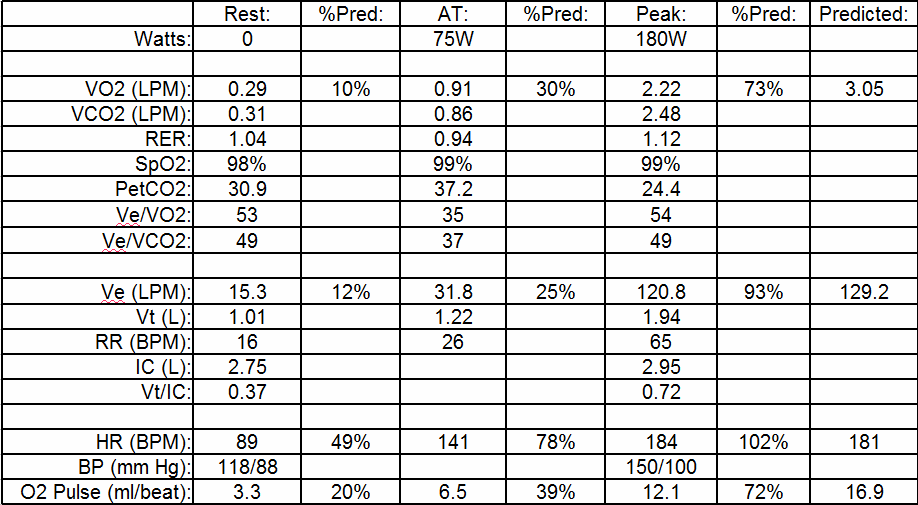
Recently I was reviewing a cardio-pulmonary exercise test (CPET) that at first glance seemed to show the patient had a pulmonary mechanical limitation. Specifically, the patient’s minute ventilation (Ve) at peak exercise was 93% of predicted. This was something you’d expect if a patient had an obstructive or restrictive lung disease but I could see right away that the patient’s baseline pulmonary function tests were actually pretty normal.
The maximum oxygen consumption was 73% of predicted so it was apparent the patient had an exercise limitation of some kind but based on a number of other factors I didn’t think it had anything to do with the mechanical aspects of the patient’s lung.
Creepy decimal points
This is one of my pet peeves. It started for me back in the 1970’s when the Intensive Care Units where I was working were evaluating thermal dilution cardiac output meters. This was at a time when digital displays were just starting to become common. One of the meters showed cardiac output with two digits after the decimal point (i.e. 0.12) and the other one had three digits after the decimal point (i.e. 0.123).
Thermal dilution cardiac output works by threading a catheter (a Swan-Ganz is what was used at the time) with a thermistor in its tip through the right side of a patient’s heart into their pulmonary artery. A small amount of iced saline is then injected through the catheter and the system times how long it takes for this cold pulse to go around the patient’s body and return. There are a number of uncertainties involved so it’s not a terribly accurate technique and the very best you could ever expect would be a precision of about 1/10th of a LPM and that’s being very generous.
We had no ability to actually determine if either meter was accurate and the best we could see was that both meters gave similar results on the same patient. Neither meter was particularly harder or easier to use than the other. Nevertheless the cardiac output meter with 3 digits after the decimal point won the evaluation hands down because everybody said it had to be more accurate. This may say something about human nature but it’s also just nonsense. Simply because somebody places extra digits after the decimal point doesn’t make the measurement more accurate.
I’ve seen many times where a test result is reported with more digits after the decimal point than you could reasonably expect to get from the equipment or the measurement. When new devices (software or smartphones for example) add new features that are of little value (other than probably as ad copy) it is called feature creep. When this happens with digits I think this should be called decimal creep.
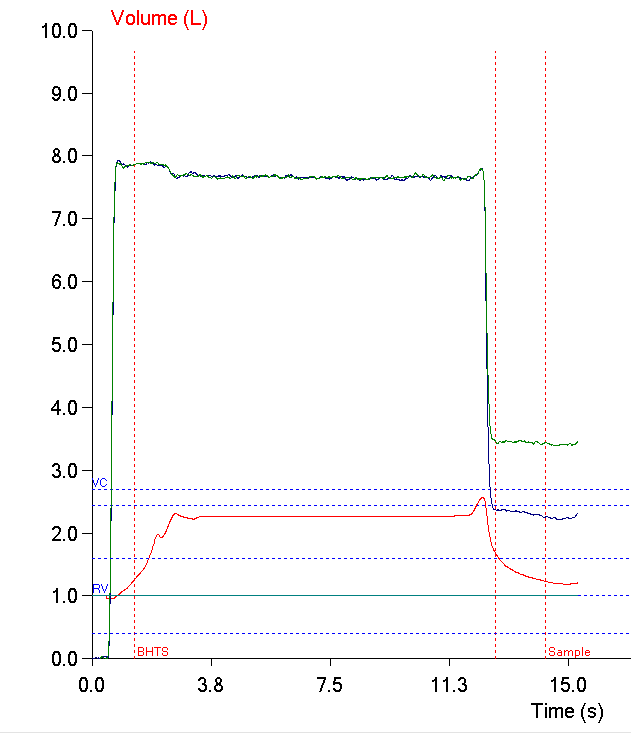
When an Inspiratory Volume really isn’t inspiring
I always like it when a patient does something during a test that makes me have to think about the basics of the test and what effect an error will have on the results. I was reviewing a report that had come across my desk and the technician performing the test had put “poor DLCO test reproducibility, fair quality in selected test” in the notes so of course I had to pull up the raw test data and take a look for myself.
The patient had performed three DLCO tests, two of which were completely unusable and one that was sort of okay but not really. Interestingly, the test system software thought it met the criteria for acceptability.
The ATS/ERS statement on DLCO testing says that the inspired volume needs to be at least 85% of the patient’s largest known vital capacity. Even though the patient’s inspired volume during most of the test was well below this threshold they made a further inspiratory effort just before exhaling and exceeded the threshold when they did. For this reason the software thought the effort was acceptable. This points out limitations in our testing system software, its hardware, and in the ATS/ERS statement as well.