My lab stopped inserting A-lines to get arterial blood samples during exercise testing well over 10 years ago. Our decision was partly based on the fact that we didn’t do them often enough to be good at it and partly based on the fact that we didn’t think that we were getting enough extra information from ABG’s to be worth the effort. Since another local hospital (a competitor but part of the same medical school network so we share pulmonary fellows with them) routinely performs level II and level III exercise tests we felt we could refer any patients that really needed ABG’s to the lab there. We don’t regret the decision and don’t feel that it has compromised the quality of our exercise testing.
Because we don’t obtain ABG’s, one of the values we don’t calculate is the deadspace/tidal volume ratio (Vd/Vt). Recently I was reading an article that related Ve-VCO2 to Vd/Vt and I was reminded of some the issues I had with Vd/Vt when I calculated it in the past. We’ve gone through two different exercise test systems since that time so I’m not sure if some of these problems still exist but I thought it would be a good idea to review both the problems and the literature on Vd/Vt to see if I could make some sense of them.
As a reminder, the original Bohr equation for Vd/Vt was:
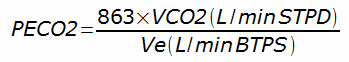
The first problem I had run into was that mixed-expired CO2 (PECO2) is routinely calculated from CPET data as:
But it was also reported as a separate value by the test system’s software and the two values did not match.